
- •Pineal Parenchymal Tumors
- •Germ Cell Tumors
- •Selected References
- •Medulloblastoma
- •Selected References
- •Anatomy of the Cranial Meninges
- •Meningomas
- •Primary Melanocytic Lesions
- •Other Related Neoplasms
- •Selected References
- •Cranial Nerve Anatomy
- •Schwannomas
- •Neurofibromas
- •Selected References
- •Histiocytic Tumors
- •Selected References
- •Sellar Region Anatomy
- •Normal Imaging Variants
- •Congenital Lesions
- •Neoplasms
- •Miscellaneous Lesions
- •Selected References
- •Intracranial Pseudotumors
- •Selected References
- •Metastatic Lesions
- •Paraneoplastic Syndromes
- •Selected References
- •Scalp Cysts
- •Extraaxial Cysts
- •Parenchymal Cysts
- •Intraventricular Cysts
- •Selected References
- •Anatomy and Physiology of the Basal Ganglia and Thalami
- •Selected References
- •Alcohol and Related Disorders
- •Opioids and Derivatives
- •Inhaled Gases and Toxins
- •Selected References
- •Selected References
- •Hypertensive Encephalopathies
- •Glucose Disorders
- •Thyroid Disorders
- •Seizures and Related Disorders
- •Miscellaneous Disorders
- •Selected References
- •The Normal Aging Brain
- •Dementias
- •Degenerative Disorders
- •Selected References
- •Normal Variants
- •Hydrocephalus
- •CSF Leaks and Sequelae
- •Selected References
- •Cerebral Hemisphere Formation
- •Imaging Approach to Brain Malformations
- •Posterior Fossa Anatomy
- •Chiari Malformations
- •Hindbrain Malformations
- •Selected References
- •Commissural Anomalies
- •Malformations Secondary to Abnormal Postmigrational Development
- •Selected References
- •Anencephaly
- •Holoprosencephaly
- •Holoprosencephaly Variants
- •Related Midline Disorders
- •Holoprosencephaly Mimics
- •Selected References
- •Selected References
- •Selected References
- •Cephaloceles
- •Craniosynostoses
- •Meningeal Anomalies
- •Selected References
- •Index

Neoplasms, Cysts, and Tumor-Like Lesions
692
Selected References
Anatomy of the Cranial Meninges
Liebo GB et al: Brain herniation into arachnoid granulations: clinical and neuroimaging features. J Neuroimaging. 26(6):592-598, 2016
Bucchieri F et al: Lymphatic vessels of the dura mater: a new discovery? J Anat. 227(5):702-3, 2015
Mortazavi MM et al: Anatomical variations and neurosurgical significance of Liliequist's membrane. Childs Nerv Syst. 31(1):15-28, 2015
Tsutsumi S et al: Cranial arachnoid protrusions and contiguous diploic veins in CSF drainage. AJNR Am J Neuroradiol. 35(9):1735- 9, 2014
Adeeb N et al: The intracranial arachnoid mater : a comprehensive review of its history, anatomy, imaging, and pathology. Childs Nerv Syst. 29(1):17-33, 2013
Adeeb N et al: The pia mater: a comprehensive review of literature. Childs Nerv Syst. 29(10):1803-10, 2013
(22-55A) Early arterial phase, lateral view of a vertebrobasilar DSA shows a patient with cerebellar hemangioblastoma. Note vascular tumor mass supplied primarily by enlarged branches of the anterior and posterior inferior cerebellar arteries. (22-55B) Late arterial phase in the same case shows the characteristic prolonged tumor "blush"coming from branches of enlarged PICA and AICA .
(22-56A) Axial T1 C+ FS in an 84y woman with a positive family history of VHL shows a cystic lesion
with an enhancing nodule in the left posteromedial temporal lobe. (22-56B) Coronal T1 C+ MR in the same case shows that the cyst wall
does not enhance, but the nodule enhances strongly, uniformly . Lesion has been stable for 5 years. This is presumed supratentorial hemangioblastoma in the setting of VHL.
Adeeb N et al: The cranial dura mater: a review of its history, embryology, and anatomy. Childs Nerv Syst. 28(6):827-37, 2012
Meningomas
Meningioma
Starr CJ et al: Meningioma mimics: five key imaging features to differentiate them from meningiomas. Clin Radiol. ePub, 2017
Zakhari N et al: Uncommon cranial meningioma: key Iimaging features on conventional and advanced imaging. Clin Neuroradiol. 27(2):135-144, 2017
Boukobza M et al: Cystic meningioma: radiological, histological, and surgical particularities in 43 patients. Acta Neurochir (Wien). 158(10):1955-64, 2016
Gerkes EH et al: A heritable form of SMARCE1-related meningiomas with important implications for follow-up and family screening. Neurogenetics. 17(2):83-9, 2016
Gunel M et al: 218Meningioma driver mutations determine their anatomical site of origin. Neurosurgery. 63 Suppl 1:185, 2016

Louis DN et al: The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 131(6):803-20, 2016
Pećina-Šlaus N et al: Molecular genetics of intracranial meningiomas with emphasis on canonical Wnt signalling. Cancers (Basel). 8(7), 2016
Perry A et al: Meningioma. In: Louis DN et al (eds), WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer, 2016, pp 232-245
Yuzawa S et al: Genetic landscape of meningioma. Brain Tumor Pathol. 33(4):237-247, 2016
Di Vitantonio H et al: Cavernous hemangioma of the dura mater mimicking meningioma. Surg Neurol Int. 6(Suppl 13):S375-8, 2015
Domingues P et al: Genetic/molecular alterations of meningiomas and the signaling pathways targeted. Oncotarget. 6(13):10671-88, 2015
Atypical Meningioma
Garzon-Muvdi T et al: Atypical and anaplastic meningioma: outcomes in a population based study. J Neurooncol. ePub, 2017
Sahm F et al: DNA methylation-based classification and grading system for meningioma: a multicentre, retrospective analysis. Lancet Oncol. 18(5):682-694, 2017
Messerer M et al: Recent advances in the management of atypical meningiomas. Neurochirurgie. 62(4):213-22, 2016
Nanda A et al: Outcome of resection of WHO Grade II meningioma and correlation of pathological and radiological predictive factors for recurrence. J Clin Neurosci. 31:112-21, 2016
Anaplastic Meningioma
Kessler RA et al: Metastatic atypical and anaplastic meningioma: a case series and review of the literature. World Neurosurg. 101:4756, 2017
Cimino PJ: Malignant progression to anaplastic meningioma: neuropathology, molecular pathology, and experimental models. Exp Mol Pathol. 99(2):354-9, 2015
Nonmeningothelial Mesenchymal Tumors
Antonescu CR et al: Mesenchymal, non-meningothelial tumors. In: Louis DN et al (eds), WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer, 2016, pp 248-254
Benign Mesenchymal Tumors
Antonescu CR et al: Mesenchymal, non-meningothelial tumors. In: Louis DN et al (eds), WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer, 2016, pp 248-254
Reinshagen C et al: Intracranial dural based chondroma. J Clin Neurosci. 25:161-3, 2016
Hemangioma
Kirmani AR et al: A unique case of calvarial hemangioma. Surg Neurol Int. 7(Suppl 14):S398-401, 2016
Wang X et al: Convexity dural cavernous haemangioma mimicking meningioma: a case report. Br J Neurosurg. 30(3):345-7, 2016
Tumors of the Meninges
693
Malignant Mesenchymal Tumors
Fathalla H et al: Osteomalacia-inducing tumors of the brain: a case report, review and a hypothesis. World Neurosurg. 84(1):189.e1-5, 2015
Solitary Fibrous Tumor/Hemangiopericytoma
Ghose A et al: CNS hemangiopericytoma: a systematic review of 523 patients. Am J Clin Oncol. 40(3):223-227, 2017
Jiang N et al: Solitary fibrous tumor of central nervous system: clinical and prognostic study of 24 cases. World Neurosurg. 99:584592, 2017
Choi J et al: Hemangiopericytomas in the central nervous system: a multicenter study of Korean cases with validation of the usage of STAT6 immunohistochemistry for diagnosis of disease. Ann Surg Oncol. 23(Suppl 5):954-961, 2016
Fritchie KJ et al: NAB2-STAT6 gene fusion in meningeal hemangiopericytoma and solitary fibrous tumor. J Neuropathol Exp Neurol. 75(3):263-71, 2016
Yalcin CE et al: Solitary fibrous tumor/hemangiopericytoma dichotomy revisited: a restless family of neoplasms in the CNS. Adv Anat Pathol. 23(2):104-11, 2016
Pang H et al: Morphologic patterns and imaging features of intracranial hemangiopericytomas: a retrospective analysis. Onco Targets Ther. 8:2169-78, 2015
Primary Melanocytic Lesions
Koelsche C et al: Melanotic tumors of the nervous system are characterized by distinct mutational, chromosomal and epigenomic profiles. Brain Pathol. 25(2):202-8, 2015
Jaiswal S et al: Primary melanocytic tumors of the central nervous system: a neuroradiological and clinicopathological study of five cases and brief review of literature. Neurol India. 59(3):413-9, 2011
Other Related Neoplasms
Hemangioblastoma
Franco A et al: CNS hemangioblastomatosis in a patient without von Hippel-Lindau disease. CNS Oncol. 6(2):101-105, 2017
Pierscianek D et al: Study of angiogenic signaling pathways in hemangioblastoma. Neuropathology. 37(1):3-11, 2017
Huntoon K et al: Biological and clinical impact of hemangioblastoma-associated peritumoral cysts in von HippelLindau disease. J Neurosurg. 124(4):971-6, 2016
Plate KH et al: Hemangioblastoma. In: Louis DN et al (eds), WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer, 2016, pp 254-257
She D et al: Differentiating hemangioblastomas from brain metastases using diffusion-weighted imaging and dynamic susceptibility contrast-enhanced perfusion-weighted MR imaging. AJNR Am J Neuroradiol. ePub, 2016
This page intentionally left blank
Chapter 23
695
Cranial Nerves and Nerve Sheath
Tumors
The 2016 WHO made relatively few changes in the way tumors of the cranial and paraspinal nerves are classified. The four basic categories of schwannoma, neurofibroma, perineurioma, and malignant peripheral nerve sheath tumor were retained. A new category, hybrid nerve sheath tumor, was added, as such histologically combined tumors are increasingly recognized by neuropathologists. Because melanotic schwannoma is both clinically and genetically distinct from "conventional" schwannoma, it is also now classified as a distinct entity rather than a variant.
With the exception of vestibular schwannoma, all intracranial nerve sheath tumors are rare. They occur ether sporadically or as part of tumor-associated familial tumor syndromes such as neurofibromatosis types 1 and 2.
The vast majority of nerve sheath neoplasms are benign. The two major tumor types that are found intracranially and at or near the skull base are schwannomas and neurofibromas. Both are discussed in detail here. The third type of benign tumor, perineurioma, is primarily a tumor of peripheral nerves and soft tissues, although rare cases involving cranial nerves have been reported. Perineurioma is briefly considered at the end of this chapter.
Malignant nerve sheath tumors—melanotic schwannoma and the rare intracranial malignant peripheral nerve sheath tumor (MPNST)—are also considered in this chapter.
More than 99% of intracranial nerve sheath tumors are associated with a cranial nerve. Because characteristic imaging findings of these tumors are location specific rather than generic, we begin this chapter with a review of normal cranial nerve anatomy.
Cranial Nerve Anatomy
In this section, we briefly cover cranial nerve (CN) anatomy, beginning our discussion with the upper cranial nerves (CNs I-VI). We then turn to the lower cranial nerves (CNs VII-XII). The function, anatomy, and key clinical/imaging points are delineated for the individual cranial nerves.
The intracranial anatomy of each nerve is discussed segment by segment, from its intraaxial location and exit from the brain, passage through the adjacent CSF cisterns, entrance into or exit from the skull base, and extracranial course. Remember: cranial nerves do not stop at the skull base! When imaging cranial neuropathies, it is critically important to image—and
Cranial Nerve Anatomy |
695 |
Upper Cranial Nerves |
696 |
Lower Cranial Nerves |
703 |
Schwannomas |
708 |
Schwannoma Overview |
708 |
Vestibular Schwannoma |
712 |
Trigeminal Schwannoma |
716 |
Jugular Foramen Schwannoma |
717 |
Facial Nerve Schwannoma |
720 |
Schwannomas of Other |
720 |
Intracranial Nerves |
|
Parenchymal Schwannomas |
721 |
Melanotic Schwannoma |
722 |
Schwannomatosis |
723 |
Neurofibromas |
723 |
Solitary Neurofibroma |
724 |
Plexiform Neurofibroma |
724 |
Malignant Nerve Sheath |
|
Neoplasms |
726 |
Malignant Peripheral Nerve |
726 |
Sheath Tumor |
|
Other Nerve Sheath Tumors |
729 |
|
|
Neoplasms, Cysts, and Tumor-Like Lesions
696
carefully evaluate—each segment, following the affected nerve all the way from its origin to its "functional endplate."
Upper Cranial Nerves
Olfactory Nerve (CN I)
Function. The olfactory nerve is a special visceral afferent involved with the sense of smell.
Anatomy. Unmyelinated fibers from bipolar receptor cells high in the nasal vault gather into fascicles, pierce the cribriform plate of the ethmoid bone, and then synapse in the olfactory bulb (23-1) (23-5). The olfactory bulb passes posteriorly to the olfactory trigone (23-4). Olfactory stria from the trigone pass into the brain with the largest tract, the lateral olfactory stria, terminating in the temporal lobe.
Olfactory nerves lack a layer of Schwann cells. Instead, special populations of glial cells called "olfactory ensheathing cells"
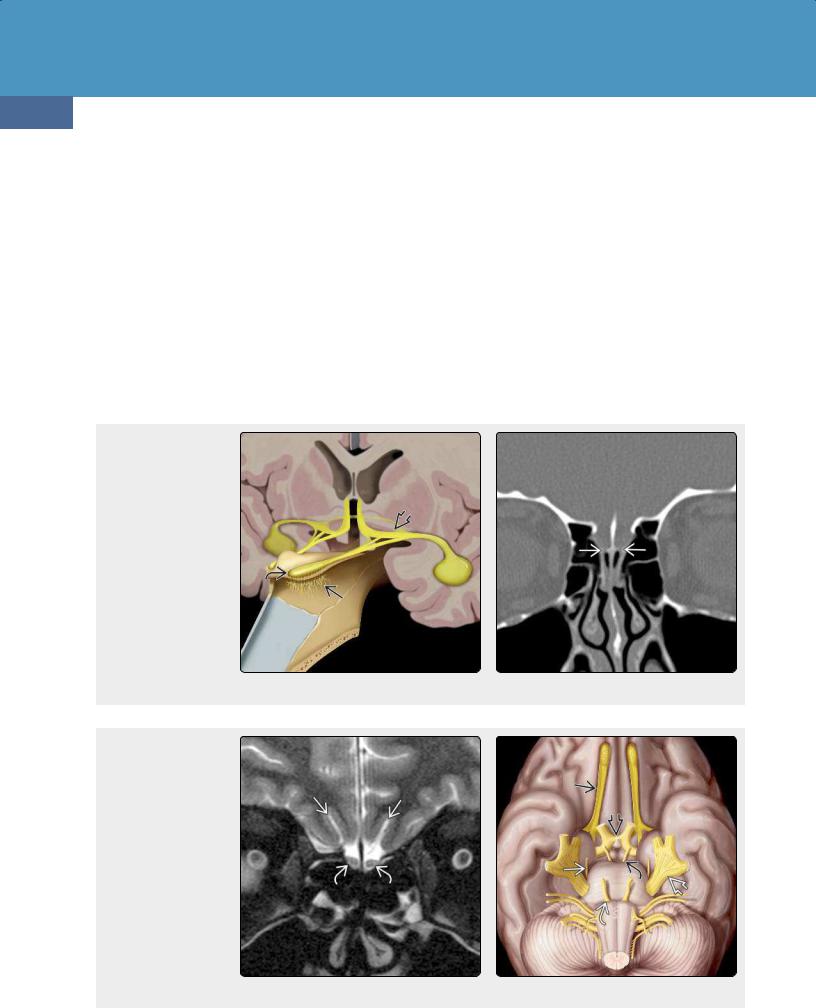
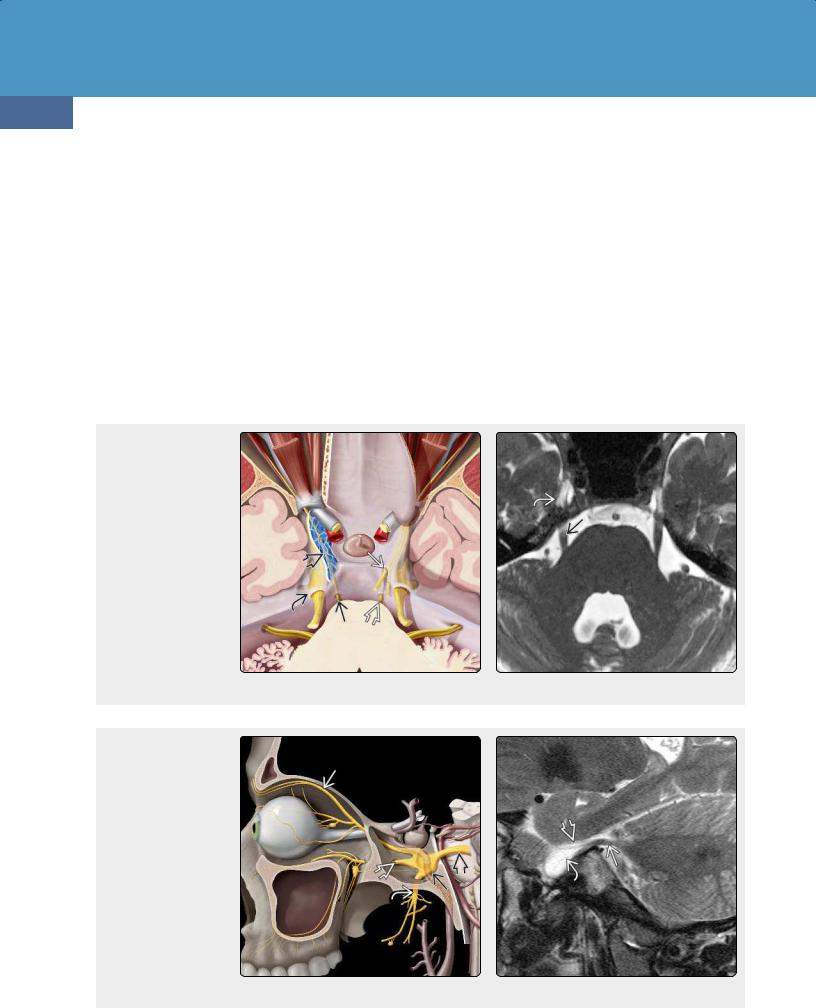
(23-1) This is cranial nerve (CN) I. Bipolar olfactory cells cross the cribriform plate and the synapse in the bulb . The olfactory tract divides into stria at the olfactory trigone . (23-2) Coronal bone CT shows the cribriform plate with fenestrations for olfactory bundles to cross from the nose to the synapse in olfactory bulbs.
(23-3) Coronal T2FS shows normal olfactory bulbs and olfactory sulci . (23-4) This graphic shows olfactory tracts (CN I) , optic chiasm , oculomotor (CN III) , trochlear (CN IV) , trigeminal , and abducens (CN VI) nerves.
(OECs) that are derived from precursor cells in the embryonic neural crest surround axons of the olfactory nerve. Similar to Schwann cells, Notch signaling pathway gene expression is important during OEC development. OECs resemble Schwann cells on light microscopy, but immunohistochemical staining distinguishes the two. OECs can both migrate and regenerate, enhancing axonal extension after injury.
Key Concepts. Coronal sinus CT that focuses on the nasal vault and cribriform plate is the best examination for isolated anosmia (23-2). MR of the nose, anterior cranial fossae, and medial temporal lobes is the best examination for clinically complicated anosmia (23-3).
Optic Nerve (CN II)
The optic nerve is technically a brain tract, not a true cranial nerve; it is ensheathed and myelinated by oligodendrocytes, not Schwann cells. Tumors of the optic nerve are
Cranial Nerves and Nerve Sheath Tumors
astrocytomas, not schwannomas, and were discussed in Chapter 17.
Function. The optic nerve is the nerve of vision.
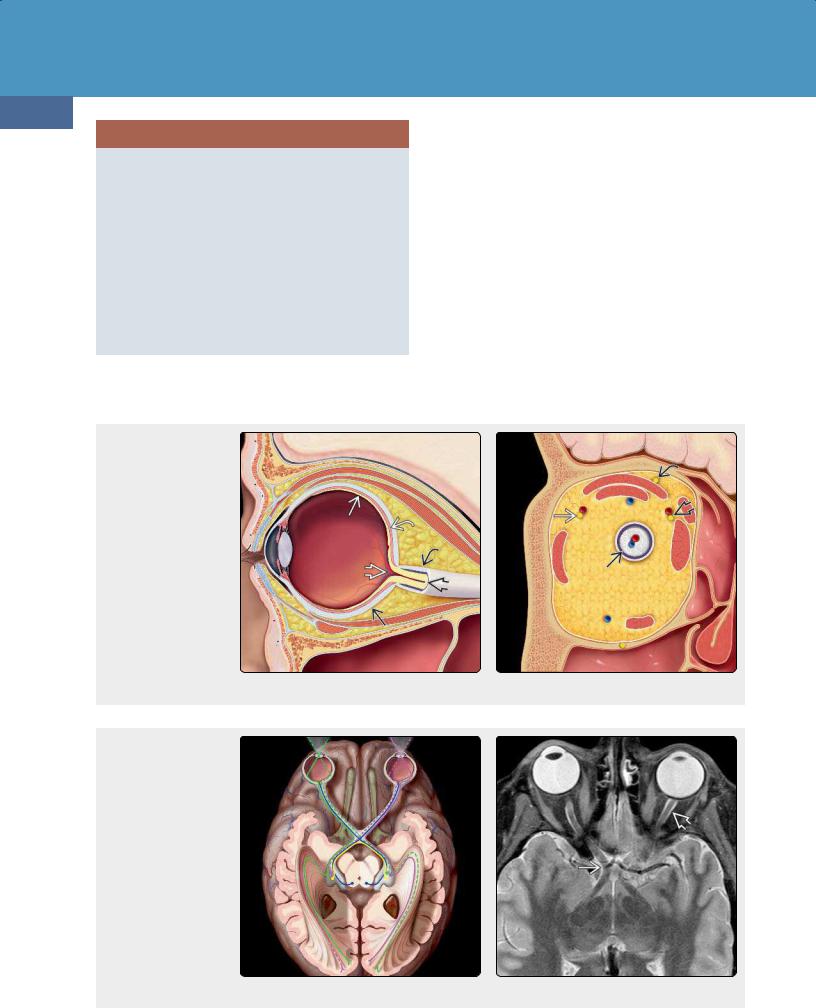
Anatomy. The visual pathway consists of the globe/retina, optic nerve, optic chiasm, and retrochiasmal structures. The intraocular segment of CN II is surrounded by a sleeve of CSF that connects directly with the intracranial subarachnoid space (SAS). It is covered by the same three meningeal layers as the brain (dura, arachnoid, pia) (23-9). The intracanalicular segment of the optic nerve passes through the optic canal
(23-5) (23-8). The intracranial (cisternal) segment extends from the optic canal to the optic chiasm.
The optic chiasm is an X-shaped structure that lies in the upper suprasellar cistern. Nerve fibers from the medial half of both retinas cross here, running posterolaterally to the opposite side (23-11) (23-12).
697
The optic tracts are posterior extensions of the optic chiasm that curve around the cerebral peduncles. Their lateral bands synapse in the lateral geniculate body (LGB). Efferent axons from the LGB form the optic radiations (geniculocalcarine tracts). The optic radiations fan out as they pass posteriorly to terminate in the calcarine cortex (primary visual cortex) along the medial occipital lobes.
Key Concepts. Globe or optic nerve pathology results in monocular visual loss. Imaging focus should extend from the globe to the optic chiasm. Intrinsic or extrinsic lesions of the optic chiasm cause bitemporal heteronymous hemianopsia, i.e., loss of both temporal visual fields. Retrochiasmal pathology causes homonymous hemianopsia, i.e., vision loss that involves either the two right or the two left halves of both visual fields. A left-sided lesion causes right homonymous hemianopsia, whereas a right-sided lesion causes left homonymous hemianopsia.
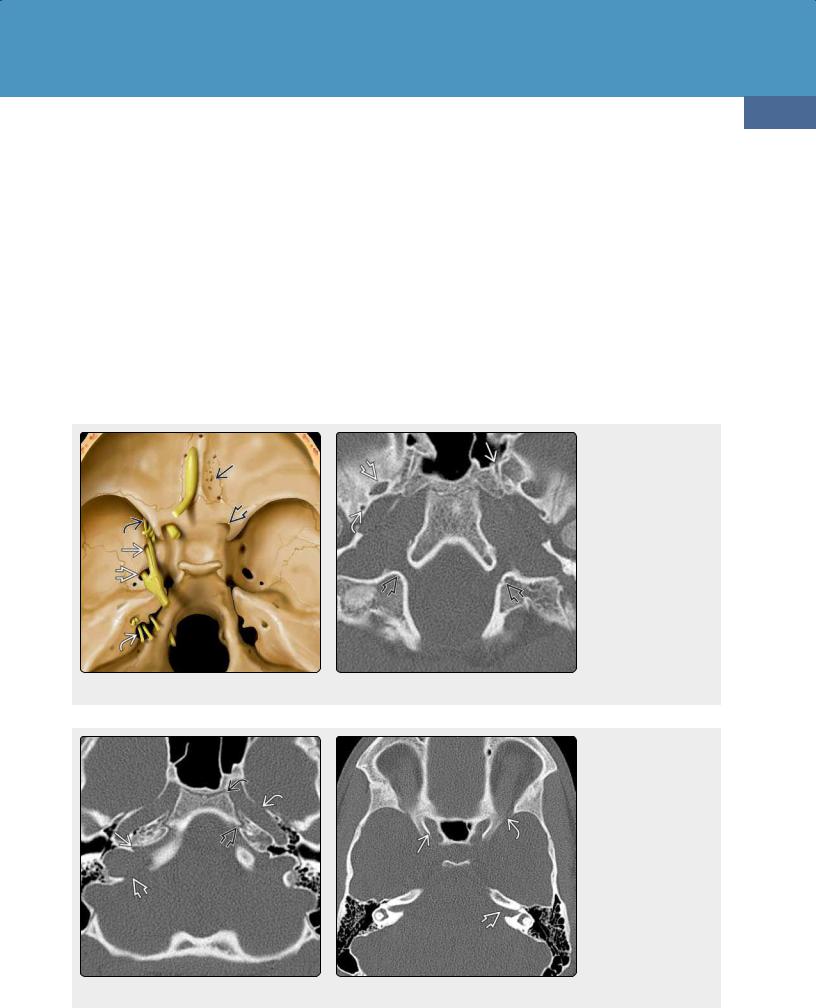
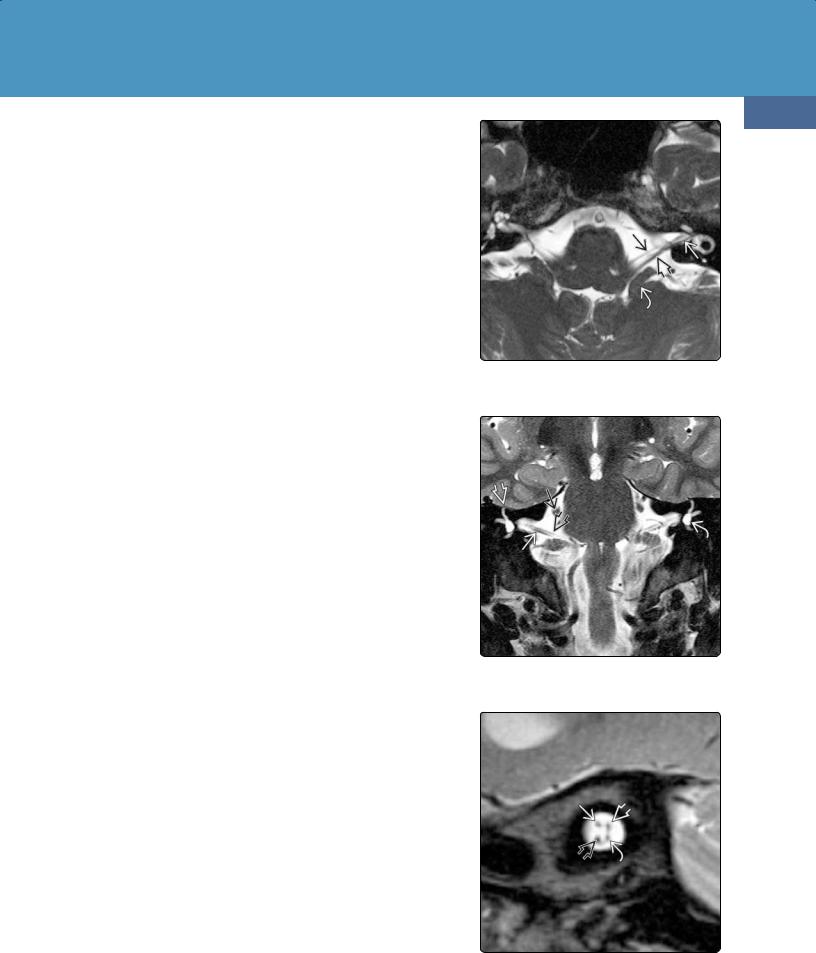
(23-5) Axial graphic depicts cranial nerves and the relationship to osseous foramina. Cribriform plate (CN I) , optic canal (CN II) , superior orbital fissure (SOF) (III, IV, V ) , rotundum (V ) , ovale (V ) , and jugular foramen (IX-XI) are shown. (23-6) Axial bone CT through the skull base shows foramen ovale (CN V ) , spinosum (middle meningeal artery) , vidian canal , and hypoglossal canals .
(23-7) Bone CT shows the jugular foramen with pars nervosa and pars vascularis . The petrous carotid canals and petro-occipital fissures are also visible. Note the presence of a sphenoccipital synchrondosis . (23-8) Bone CT shows the optic canals and internal auditory canals . The section is through the most cephalad aspect of the superior orbital fissures, which are barely visible .
Neoplasms, Cysts, and Tumor-Like Lesions
698
UPPER CRANIAL NERVES I AND II
Olfactory Nerve (CN I)
•Function = visceral afferent for smell
•Skull entrance = cribriform plate
•Key concept
○Image the coronal plane from upper nose to temporal lobes
Optic Nerve (CN II)
•Function = vision
•Skull entrance = optic canal
•Key concepts
○Myelinated brain tract
○Not ensheathed by Schwann cells
○Tumors are astrocytomas, not schwannomas
Papilledema is the ocular manifestation of increased intracranial pressure that is transmitted along the SAS of the
(23-9) Sagittal graphic depicts the globe with the optic nerve inside its dura-arachnoid sheath . The retina , choroid , sclera , and central retinal artery/vein are illustrated. The two extraocular muscles just under the orbital roof are the levator palpebrae and superior rectus. The inferior rectus is depicted below. (23-10) Coronal graphic shows optic nerve, IV frontal nerve (CN V ) , and the abducens nerve .
(23-11) Graphic depicts the visual system with the fields from the globes to the calcarine cortex. (2312) Axial T2WI shows optic nerves surrounded by CSF in optic nerve sheath . Optic chiasmand tracts are also visible.
optic nerve sheath complex. On imaging studies with moderate to severe papilledema, the posterior sclerae become flattened, and the optic nerve head may appear elevated. Accentuated tortuosity and elongation with dilatation of the perioptic SAS are common.
Oculomotor Nerve (CN III)
Function. The oculomotor nerve has both motor and parasympathetic functions. It innervates all the extraocular muscles except the lateral rectus and superior oblique muscles. Its parasympathetic fibers control pupillary sphincter function and accommodation.
Anatomy. The oculomotor nerve has four segments. Its intraaxial segment is in the midbrain. The oculomotor nucleus lies just in front of the periaqueductal gray matter. The fascicles of CN III course anteriorly through the red nucleus and substantia nigra, then exit the midbrain medial to the cerebral peduncles (23-4).

Cranial Nerves and Nerve Sheath Tumors
The cisternal segment courses anteriorly toward the cavernous sinus, passing between the posterior cerebral and superior cerebellar arteries.
The intracavernous segment lies in the superolateral wall of the cavernous sinus and is surrounded by a thin sleeve of CSF (the oculomotor cistern) (23-13) (23-15) (23-16). The oculomotor nerve exits the cavernous sinus through the superior orbital fissure (23-5). Its extracranial segment passes through the tendinous annulus and then divides into superior and inferior branches. Preganglionic parasympathetic fibers follow the inferior branch to the ciliary ganglion.
Key Concepts. The pupilloconstrictor fibers of CN III are located in the periphery of the nerve, predominantly along its superolateral aspect. The cisternal segment of the oculomotor nerve lies in close proximity to the posterior communicating artery (PCoA). PCoA aneurysms often compress the third nerve, causing a pupil-involving third nerve palsy. Pupil-sparing third nerve palsy is commonly
699
caused by microvascular infarction of the core of the nerve with relative sparing of its peripheral fibers.
Trochlear Nerve (CN IV)
Function. The trochlear nerve is a pure motor nerve that innervates the superior oblique muscle.
Anatomy. Like the oculomotor nerve, CN IV has four segments. Its intraaxial segment is also in the midbrain, anterior to the periaqueductal gray matter lying just below the oculomotor nerve nuclei. Its fascicles then course posteroinferiorly around the cerebral aqueduct and decussate within the superior medullary velum. The trochlear nerve exits the dorsal midbrain just below the inferior colliculi (23-14).
The cisternal segment courses anteriorly in the ambient cistern, adjacent to the free edge of the tentorium. It then passes between the posterior cerebral and superior cerebellar arteries, just inferior to the oculomotor nerve, and enters the
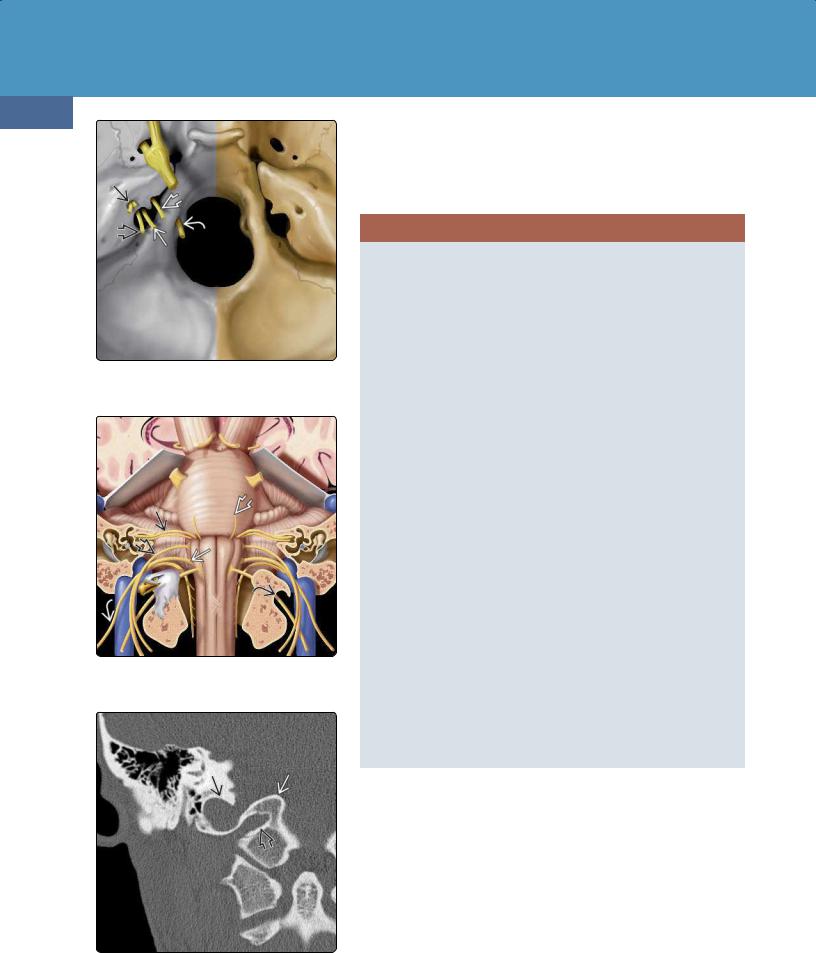
(23-13) Graphic shows oculomotor nuclei in midbrain (green) and nerve exiting between posterior and superior cerebellar arteries at interpeduncular fossa and coursing through CSFfilled oculomotor cistern in cavernous sinus to enter the orbit through the SOF . (23-14) Graphic shows trochlear nuclei , dorsally exiting and decussating trochlear nerves , trigeminal nerve (CN V) , CN IV in cavernous sinus and orbit.
(23-15) Except CN VI , cavernous sinus CNs are in lateral dural wall. CNs III surrounded by CSF-filled oculomotor cistern , IV, V , and V are shown. Optic tracts pass posteriorly from chiasm and curve around hypothalamus. (23-16) Coronal T2 shows CN III in the CSF-filled oculomotor cistern , fascicles of trigeminal nerve in Meckel cave , and gasserian ganglion . Optic chiasmis seen in suprasellar cistern.
Neoplasms, Cysts, and Tumor-Like Lesions
700
cavernous sinus (CS). The cavernous segment lies in the lateral dural wall, just below CN III (23-15).
The trochlear nerve exits the CS through the superior orbital fissure together with CNs III and VI. The extracranial segment then passes above the tendinous annulus of Zinn (CNs III and VI pass through the ring) (23-14).
Key Concepts. The long course of the cisternal segment and its proximity to the hard knife-like edge of the tentorium make the trochlear nerve especially vulnerable to injury during closed head trauma. Trochlear palsy causes superior oblique paralysis, resulting in outward rotation (extorsion) of the affected eye. The resulting diplopia and weakness of downward gaze causes most patients to compensate by tilting their heads away from the affected side. Look for trochlear neuropathy in patients with torticollis ("wry neck").
(23-17) Axial graphic shows abducens nerve (CN VI) exiting at pontomesencephalic junction, coursing across the prepontine cistern to Dorello canal , ascending under the dura to cross the petrous apex, and course through the cavernous sinus to the SOF. CN V in Meckel cave, CN III , and CN IVare also shown. (2318) Axial T2WI shows the cisternal and Meckel cave segments of the trigeminal nerve.
(23-19) Graphic shows trigeminal nerve branches V , V , and V , cisternal segment , and the gasserian ganglion in Meckel cave . (23-20) Sagittal T2 FS MR shows the trigeminal nerve trunkas it crosses the cerebellopontine angle (CPA) cistern toward the pons. Meckel cave is CSFfilled and is continuous with the CPA cistern. Note individual nerve fascicles of CN V within Meckel cave.
Trigeminal Nerve (CN V)
Function. The trigeminal nerve is a mixed sensory and motor nerve. It is the major sensory nerve of the head and face and innervates the muscles of mastication.
Anatomy. The trigeminal nerve has four segments: a ganglion (the semilunar ganglion) and three postganglionic divisions
(23-19).
The intraaxial segment has four nuclei (three sensory and one motor) that are located in the brainstem and upper cervical spinal cord (between C2 and C4).
CN V emerges from the lateral pons at the root entry zone. The cisternal segment courses anteriorly through the prepontine cistern. It then passes through a dural ring, the porus trigeminus, to enter Meckel cave (23-17) (23-18).
The interdural segment lies entirely within Meckel cave, a CSF-filled, dura-arachnoid-lined outpouching from the

Cranial Nerves and Nerve Sheath Tumors
prepontine SAS. Once inside Meckel cave, CN V separates into several discrete fascicles (23-16) (23-20). It then synapses in the trigeminal (gasserian or semilunar) ganglion, a small crescent of tissue that lies at the bottom of Meckel cave.
The postganglionic segment of CN V consists of three divisions: CN V (ophthalmic nerve), CN V (maxillary nerve), and CN V (mandibular nerve).
The ophthalmic nerve lies in the lateral cavernous sinus wall just below CN IV. It passes anteriorly toward the orbital apex and exits the CS through the superior orbital fissure. The ophthalmic nerve is a pure sensory nerve, innervating the scalp, forehead, nose, and globe.
The maxillary nerve courses anteriorly in the lateral dural wall of the CS, just below CN V . It exits through the foramen rotundum, traversing the upper aspect of the pterygopalatine fossa. It enters the orbit and courses anteriorly in the infraorbital groove, exiting through the infraorbital foramen.
701
The maxillary nerve supplies sensation to the cheek and upper teeth.
The mandibular nerve exits Meckel cave directly from the semilunar ganglion, passing inferiorly through the foramen ovale. Unlike the other two postganglionic divisions, CN V does not pass through the CS. The mandibular nerve is both motor and sensory, supplying the muscles of mastication, the mylohyoid, and the anterior belly of the digastric. Its most important sensory innervations involve the teeth and tongue.
Key Concepts. Be alert for denervation atrophy (shrinkage, fatty infiltration) of the muscles of mastication. That may be the first imaging indication of CN V neuropathy and should prompt further evaluation. (Meckel cave lesions are a common cause.)
(23-21) CN VI nerve/nucleus is shown. CN VII nuclei/internal auditory canal (IAC) segment , geniculate ganglion , greater superficial petrosal nerve (GSPN) , and CN VIII cochlear and vestibular nerves can all be seen. (23-22) Axial T2WI at the level of the pontomedullary junction shows the right VI nerve and the left CN VI as it heads into Dorello canal. The cochlear nerve is also well seen on this image.
(23-23) Sagittal T2WI shows CN VI as it exits anteriorly from the pontomedullary junctionand crosses the prepontine cistern toward Dorello canal. (2324) T2WI shows left CN VIand VII , vestibulocochlear , and superior vestibular nerves, and right cochlear , inferior vestibular nerves.

Neoplasms, Cysts, and Tumor-Like Lesions
702
Abducens Nerve (CN VI)
Function. The abducens nerve is a pure motor nerve. It provides innervation to the lateral rectus muscle (abduction).
Anatomy. The abducens nerve has five segments. The intraaxial segment begins in the CN VI nuclei, which are located in the pons, just anterior to the fourth ventricle. Axons of CN VII loop around the abducens nuclei, creating the "bump" in the floor of the fourth ventricle called the facial colliculus (23-21).
Fibers from the abducens nuclei course directly anteriorly, emerging from the brainstem just lateral to the midline at the pontomesencephalic junction.
The cisternal segment of CN VI ascends anterosuperiorly through the prepontine cistern, then penetrates the clival dura (23-17) (23-23). The interdural segment of CN VI courses superiorly between the two layers of dura in a shallow
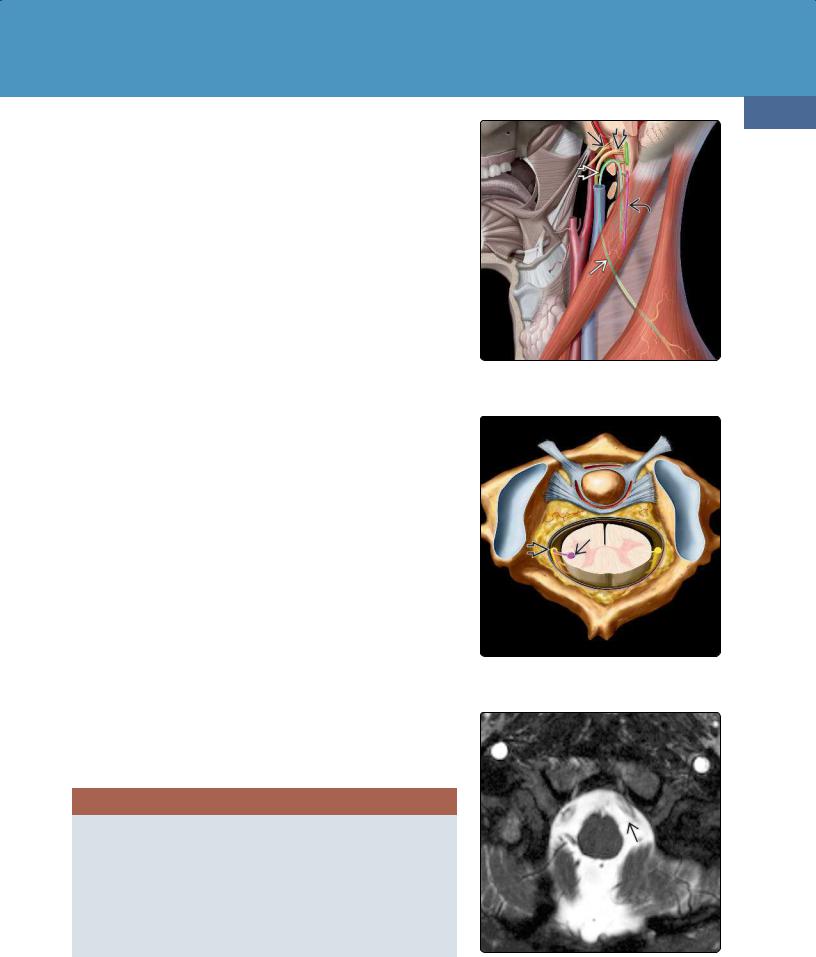
(23-25) CN VII GSPN , chorda tympani , stapedius nerve , and stylomastoid foramen are all shown. Distal branches ramify within the parotid gland. (23-26) Solitary nucleus to chorda tympani (taste) , superior salivatory nucleus to GSPN (lacrimation) , and motor nucleus/nerve are all shown in this graphic.
(23-27) Bone CT shows tympanic segment under lateral semicircular canal and the mastoid segment descending to the stylomastoid foramen. (23-28) Axial temporal bone CT shows the bony labyrinthine segment of CN VII and its anterior genu for the geniculate ganglion .
channel known as Dorello canal. The abducens nerve then crosses over the top of the petrous apex just below the petrosphenoidal ligament to enter the CS.
The cavernous segment courses anteriorly within the CS itself, the only cranial nerve to do so (the others are embedded within the lateral dural wall). Inside the CS, the abducens nerve lies along the inferolateral aspect of the internal carotid artery (23-15).
CN VI exits the CS through the superior orbital fissure. The intraorbital segment passes anteriorly through the tendinous ring that attaches the extraocular muscles.
Key Concepts. Simple (i.e., isolated) abducens palsy is the most common ocular motor nerve palsy. A "pseudo" sixth nerve palsy (inability to abduct the eye) is usually caused by an infiltrative lesion in the lateral rectus muscle itself.

Cranial Nerves and Nerve Sheath Tumors
In its course over the petrous apex, the abducens nerve is vulnerable to increased intracranial pressure and inflammation in the adjacent temporal bone ("apical petrositis").
UPPER CRANIAL NERVES III-VI
Oculomotor Nerve (CN III)
•Function
○Innervates all extraocular muscles, except lateral rectus, superior oblique
•Skull exit = superior orbital fissure (SOF)
•Key concept
○Is neuropathy pupil-involving or pupil-sparing?
Trochlear Nerve (CN IV)
•Function = innervates superior oblique muscle
•Skull exit = SOF
•Key concept
○Head tilt/torticollis can be caused by CN IV injury
Trigeminal Nerve (CN V)
•Function (mixed motor, sensory)
○Innervates muscles of mastication
○Sensory from head, face
•Skull exits
○Ophthalmic (CN V ) = SOF
○Maxillary (CN V ) = foramen rotundum
○Mandibular (CN V ) = foramen ovale
•Key concepts
○Look at face!
○Denervation atrophy of masticator muscles
Abducens Nerve (CN VI)
•Function = innervates lateral rectus
•Skull exit = SOF
•Key concepts
○Intrinsic lateral rectus disease can mimic CN VI palsy
○↑ Intracranial pressure, apical petrositis can cause abducens palsy
Lower Cranial Nerves
Facial Nerve (CN VII)
Function. The facial nerve has multiple functions. It provides motor innervation to the muscles of facial expression. It provides parasympathetic innervation to the lacrimal, submandibular, and sublingual glands. It also provides a special sensory function, i.e., taste, to the anterior two-thirds of the tongue.
Anatomy. The facial nerve has four segments. The intraaxial segment consists of the facial nerve nuclei that lie in the ventrolateral pons. Efferent fibers from the motor nucleus loop dorsally around the abducens nucleus, then pass anterolaterally to exit the brainstem at the pontomedullary junction (23-21).
The cisternal segment of CN VII courses laterally through the cerebellopontine angle (CPA) together with the vestibulocochlear nerve (CN VIII) to the internal auditory canal (IAC) (23-24).
703
The intratemporal facial nerve follows a complex course, first coursing laterally as the IAC segment and the most anterosuperior of the four nerves within the IAC (23-30) (2334). It then exits the bony IAC, bending anteriorly and becoming the labyrinthine segment. At its most anterior bend (which is called the "anterior genu"), the facial nerve synapses in the geniculate ganglion and then courses posteriorly under the lateral semicircular canal as the tympanic segment (23-25) (23-28). It curves inferiorly at the "posterior genu" and descends in the mastoid as the mastoid segment (23-27).
The important intratemporal branches of the facial nerve from top to bottom are the greater superficial petrosal nerve (parasympathetic fibers that supply the lacrimal gland), the stapedius nerve (innervation of the stapedius muscle), and the chorda tympani (taste from the anterior two-thirds of the tongue) (23-26).
The facial nerve exits the skull at the stylomastoid foramen, then enters the parotid gland. Once inside the gland, the extracranial facial nerve ramifies into its terminal motor branches, which innervate the muscles of facial expression
(23-25).
Key Concepts. Facial nerve enhancement within the CPA cistern or IAC is always abnormal. With the exception of the labyrinthine segment, a robust vascular plexus surrounds most of the intratemporal facial nerve. Therefore, the facial nerve is the only cranial nerve with segments that may exhibit some enhancement following contrast administration.
If the bony intratemporal CN VII canal is normal, mild enhancement of the geniculate ganglion and tympanic and mastoid segments is considered normal. The geniculate ganglion enhances in 75% of cases, and tympanic segment enhancement occurs in half of all cases. The mastoid segment nearly always enhances. Segmental facial nerve enhancement is more conspicuous at higher field strengths (3.0 T).
The first step in facial nerve imaging requires clinical input. When imaging is requested for "facial nerve palsy," detailed information is key. Typical Bell palsy (i.e., of short duration, uncomplicated by other CN neuropathy) does not need imaging.
It is essential to know whether a facial nerve deficit is central ("upper motor neuron") or peripheral ("lower motor neuron"). Upper (central or supranuclear) motor neuron injury, due to a parenchymal lesion above the brainstem, results in paralysis of the contralateral muscles of facial expression but spares the forehead. Stroke is a common cause of upper motor neuron facial palsy.
Lower motor neuron injury can involve CN VII at any point from its brainstem nucleus through its peripheral branches. Lower motor neuron facial palsy involves paralysis of all ipsilateral muscles of facial expression. In such cases, imaging should extend from the brainstem through the parotid gland.
If a lower motor neuron facial injury is present, further information regarding the so-called special functions of the facial nerve is essential. Are taste and lacrimation intact? Does

Neoplasms, Cysts, and Tumor-Like Lesions
704
(23-29) CN VIII. Cochlear nerve/modiolus , inferior /superior vestibular nerves, nuclei in medulla, tracts in inferior cerebellar peduncle.
(23-30) Bony IAC with facial nerve (CN VII) , cochlear nerve (CN VIII) , superior /inferiorvestibular nerves, crista falciformis .
(23-31) Cochlea with modiolus , cochlear nerve, and aperture . Spiral ganglion cells are shown in yellow within the modiolus.
the patient have hyperacusis? If these special functions are spared, the cause of a lower motor neuron facial palsy is extracranial.
If the special functions are affected, knowing exactly which ones are involved helps localize lesion extent. Malignant parotid tumors—especially adenoid cystic carcinoma—have a marked propensity to enter the stylomastoid foramen and invade up the intratemporal facial nerve.
The most distal of the intratemporal facial nerve branches is the chorda tympani, which is affected first. Loss of taste in the anterior tongue results. As tumor progresses more cephalad, the next affected branch is the stapedius nerve. Hyperacusis results. As tumor reaches the geniculate ganglion, the greater superficial petrosal nerve is compromised, resulting in problems with lacrimation.
A lesion proximal to the geniculate ganglion will cause facial paralysis and affect all three special functions.
If a complete lower neuron facial palsy is complicated by CN VI and/or CN VIII involvement, the lesion is most likely in the pons (CN VI) or CPA-IAC (CN VIII).
CRANIAL NERVES VII AND VIII
Facial Nerve (CN VII)
•Functions
○Motor (muscles of facial expression)
○Special sensory (taste, anterior 2/3 of tongue)
○Parasympathetics (lacrimal, submandibular, sublingual glands)
•Skull exit
○Exits through stylomastoid foramen into IAC along with CN VIII
•Key concepts
○Typical Bell palsy does not require imaging
○CN VII neuropathy? Ask if upper or lower motor neuron
○Parotid malignancies "creep up" facial nerve
○Special functions affected (taste, hyperacusis, lacrimation)?
Vestibulocochlear Nerve (CN VIII)
•Function = afferent sensory nerve
○Hearing (cochlear nerve)
○Balance (vestibular nerve)
•Skull entrance = internal auditory canal
○Most anteroinferior = cochlear nerve
○Posterior = superior, inferior vestibular nerves
•Key concepts
○MR in vestibular nerve dysfunction usually negative
○Unilateral sensorineural hearing loss with lesion on MR → 95% vestibulocochlear schwannomas
Vestibulocochlear Nerve (CN VIII)
Function. The vestibulocochlear nerve is purely sensory. It is the afferent sensory nerve responsible for hearing and the sense of balance.
Anatomy. CN VIII has two major components, the cochlear nerve and the vestibular nerve (23-29) (23-30). Unlike the other cranial nerves, CN VIII is best described from outside to inside (peripheral to central).
The cochlear nerve arises from the spiral ganglion in the modiolus of the cochlea. Its fibers pass through the cochlear aperture into the IAC (23-31). The cochlear nerve is the most anteroinferior of the four nerves in the IAC (23-34). Near the opening of the IAC, the porus acusticus, the cochlear nerve joins the superior and inferior vestibular nerves to form the vestibulocochlear nerve.
Cranial Nerves and Nerve Sheath Tumors
The vestibular nerve arises from bipolar neurons in the vestibular ganglion at the IAC fundus. Its fibers coalesce to form the superior and inferior vestibular nerves, which are separated by a bony bar called the falciform (transverse) crest. The superior and inferior vestibular nerves course medially in the posterior aspect of the IAC (23-32) (23-33). At the porus acusticus, they join with the cochlear nerve to form CN VIII.
CN VIII passes medially through the CPA cistern and enters the lateral brainstem at the pontomedullary junction to become the intraaxial segment. The cochlear nuclei are found in the restiform body at the lateral surface of the inferior cerebellar peduncle. The vestibular nuclei lie along the inferior floor of the fourth ventricle.
Key Concepts. At least 90-95% of all lesions that cause unilateral sensorineural hearing loss—and are detected on imaging—are vestibulocochlear schwannomas. Isolated vestibular nerve dysfunction (dizziness, vertigo, balance problems) usually does not have positive findings on MR. "Conductive" (intracochlear) hearing loss is best evaluated by highresolution multiformatted temporal bone CT.
Glossopharyngeal Nerve (CN IX)
Function. The glossopharyngeal nerve is small but has complex functions. It is a special sensory nerve (responsible for taste in the posterior third of the tongue) as well as a regular sensory nerve (innervating middle ear, pharynx). It carries parasympathetic fibers to the parotid gland and is the motor supply to the stylopharyngeus muscle. Last but by no means least, it is viscerosensory to the carotid body and sinus.
Anatomy. Like most of the other cranial nerves, CN IX has four segments: intraaxial, cisternal, skull base, and extracranial.
CN IX has four nuclei. All are in the upper and middle medulla, anterolateral to the inferior fourth ventricle. The intraaxial segment consists of these nuclei plus their tracts. The tracts course anterolaterally from the nuclei to exit or enter the medulla in the postolivary sulcus.
The cisternal segment travels toward the jugular foramen, coursing just above the vagus nerve. The glossopharyngeal nerve exits the skull by passing into the anterior aspect (pars nervosa) of the jugular foramen (23-7) (2335). In its skull base segment, the glossopharyngeal nerve lies adjacent to the inferior petrosal sinus. Its extracranial segment courses inferiorly through the carotid space.
Key Concepts. In the coronal plane, the jugular tubercles and basiocciput form a construct that resembles the head, beak, and body of an eagle. CN IX (together with CNs X and XI) courses through the jugular foramen, which lies superolateral to the eagle's "head" and "beak." The hypoglossal canal lies under the eagle's "head," at the "neck" formed by the "beak" above and the "body" below (23-36) (23-37).
Vagus Nerve (CN X)
Function. The vagus nerve is also a mixed nerve with sensory (ear, larynx, viscera), special (taste from epiglottis), motor (most of soft palate, superior and recurrent laryngeal nerves), and parasympathetic (regions of head/neck, thorax, abdominal viscera) functions.
Anatomy. The intraaxial segment of the vagus nerve lies in the inferior medulla. Its nuclei lie in front of the inferior fourth ventricle. Fibers to and from the nuclei exit the medulla in the postolivary sulcus. Its cisternal segment courses anterolaterally through the medullary cistern, lying between the glossopharyngeal nerve above and the bulbar portion of the spinal accessory nerve (CN XI) below.
705
(23-32) Axial T2WI shows CN VII , vestibulocochlear nerve (CN VIII) , superior vestibular nerve , flocculus of cerebellum .
(23-33) Coronal T2WI shows CN V , CN VII , CN VIII , vestibule , and superior semicircular canal .
(23-34) Sagittal T2WI of mid IAC shows 4 nerves as "dots" in CSF: CN VII , superior and inferior vestibular nerves, cochlear nerve .
Neoplasms, Cysts, and Tumor-Like Lesions
706
(23-35) Lower CNs, foramina are shown: CNs VII and VIII in IAC , CNs IX , X , XI in jugular foramen, CN XII in hypoglossal canal.
(23-36) CNs VI , VII, VIII , IX , X , XI , and XII are shown. Jugular tubercle looks like the head of an eagle.
Its skull base segment begins where CN X enters the posterior aspect (pars vascularis) of the jugular foramen. It lies anteromedial to the jugular bulb. CN X exits the jugular foramen into the carotid space. It descends, passing under the aortic arch on the left and the subclavian artery on the right. The recurrent laryngeal nerves on both sides then turn cephalad to course superiorly in the tracheoesophageal groove.
CRANIAL NERVES IX, X, AND XI
Glossopharyngeal Nerve (CN IX)
•Functions
○Taste/sensation to posterior 1/3 of tongue
○Sensory to middle ear/pharynx
○Parasympathetic to parotid gland
○Motor to stylopharyngeus
○Viscerosensory to carotid body/sinus
•Skull exit
○Jugular foramen (pars nervosa)
•Key concepts
○Isolated CN IX neuropathy very rare
○Usually occurs with CNs X, XI neuropathy
○Look for medullary cistern, skull base lesion
Vagus Nerve (CN X)
•Functions
○Sensory (ear, larynx, viscera)
○Taste (epiglottis)
○Motor (innervates soft palate, pharyngeal constrictors, larynx)
○Parasympathetic (head/neck, thorax, abdomen)
•Skull exit
○Jugular foramen (pars vascularis)
•Key concepts
○Proximal neuropathy: image medulla to hyoid
○Distal neuropathy: image through subclavian artery (right), aortopulmonary window (left)
Spinal Accessory Nerve (CN XI)
•Function
○Motor to sternomastoid, trapezius
•Skull exit/entrance
○Spinal component enters through foramen magnum
○Unites with bulbar portion
○Both exit through jugular foramen (pars vascularis)
•Key concepts
○May be injured during radical neck dissection
○Look for ipsilateral trapezius atrophy
Key Concepts. Proximal vagal neuropathy requires imaging from the medulla to the level of the hyoid. If multiple cranial nerves (CNs IX-XII) are affected, the culprit lesion is usually in the medullary cistern or skull base (jugular foramen), where all four nerves are in close proximity.
Distal vagal neuropathy is usually isolated and manifests as laryngeal dysfunction (look for a paramedian vocal cord). It requires imaging from the level of the hyoid all the way to the carina/aortopulmonary window on the left and the subclavian artery on the right.
Spinal Accessory Nerve (CN XI)
(23-37) CNs IX/X/XI exit jugular foramen on top of jugular tubercle (eagle's "head"). CN XII exits hypoglossal canal under eagle's "beak."
Function. The spinal accessory nerve is a pure motor nerve that innervates the sternomastoid and trapezius muscles.
Cranial Nerves and Nerve Sheath Tumors
Anatomy. CN XI has two intraaxial segments that arise from two different sets of nuclei, one in the medulla and the other in the proximal cervical cord. Bulbar fibers arise from the nucleus ambiguus in the medulla (23-38). Spinal fibers originate from the spinal nucleus, a column of cells along the anterior horn extending from C1-C5 (23-39).
The two cisternal segments of CN XI initially follow different courses. The bulbar fibers exit the medulla at the postolivary sulcus (23-40) and course anterolaterally through the basal cistern together with CNs IX and X. The spinal fibers emerge from the lateral aspect of the cervical spinal cord and course superiorly (23-41). Both fiber bundles then unite in the basal cistern. The skull base segment of CN XI passes through the posterior part (pars vascularis) of the jugular foramen, together with the vagus nerve and jugular bulb (23-44).
The extracranial segment begins as the glossopharyngeal nerve exits the jugular foramen into the carotid space.
Key Concepts. CN XI is often injured during radical neck dissection. Look for trapezius atrophy and compensatory hypertrophy of the ipsilateral levator scapulae.
707
(23-38) CNs IX , X , XI . Bulbar CN XI crosses to CN X and joins spinal root from spinal accessory nucleus of CN XI in jugular foramen.
Hypoglossal Nerve (CN XII)
Function. The hypoglossal nerve is a pure motor nerve that innervates both the intrinsic and most of the extrinsic (styloglossus, hyoglossus, genioglossus) tongue muscles. The only exception is the geniohyoid muscle, which is innervated by the C1 spinal nerve.
Anatomy. The hypoglossal nerve has four distinct segments. The intraaxial, cisternal, and skull base segments are relatively short. The extracranial segment is by far the longest and most complex portion of CN XII.
The intraaxial segment of CN XII begins at the hypoglossal nucleus. The hypoglossal nucleus lies just under the hypoglossal eminence of the inferior fourth ventricle. Fibers course anteriorly across the medulla and exit at the preolivary (ventrolateral) sulcus to enter the medullary (basal) cistern.
The cisternal segment extends from its exit at the medulla through the basal cistern to the entrance of the hypoglossal canal (23-41). Accompanied by a prominent venous plexus, the skull base segment of CN XII passes through the hypoglossal canal, which is located in the occipital bone beneath the jugular tubercle and jugular foramen (23-42) (23-43).
The extracranial segment of the hypoglossal nerve descends in the posterior aspect of the carotid space. It exits the carotid space between the carotid artery and the internal jugular vein, then runs anteroinferiorly toward the hyoid bone to provide motor innervation to the tongue muscles.
HYPOGLOSSAL NERVE (CN XII)
Function
• Motor to tongue muscles
Skull Exit = Hypoglossal Canal
•At base of occipital bone
•Below jugular tubercle, jugular foramen
Key Concepts
•Look for ipsilateral denervation tongue atrophy
•Shrunken, fatty infiltration
Key Clinical/Imaging Concepts. CN XII is most readily identified on axial images. The clival cortex takes an abrupt right-angle turn anterolaterally and
(23-39) The spinal nucleus of CN XI sends rootlets to form the spinal root of the accessory nerve .
(23-40) Axial T2WI demonstrates the left bulbar CN XI segment exiting the postolivary sulcus.
