
- •Pineal Parenchymal Tumors
- •Germ Cell Tumors
- •Selected References
- •Medulloblastoma
- •Selected References
- •Anatomy of the Cranial Meninges
- •Meningomas
- •Primary Melanocytic Lesions
- •Other Related Neoplasms
- •Selected References
- •Cranial Nerve Anatomy
- •Schwannomas
- •Neurofibromas
- •Selected References
- •Histiocytic Tumors
- •Selected References
- •Sellar Region Anatomy
- •Normal Imaging Variants
- •Congenital Lesions
- •Neoplasms
- •Miscellaneous Lesions
- •Selected References
- •Intracranial Pseudotumors
- •Selected References
- •Metastatic Lesions
- •Paraneoplastic Syndromes
- •Selected References
- •Scalp Cysts
- •Extraaxial Cysts
- •Parenchymal Cysts
- •Intraventricular Cysts
- •Selected References
- •Anatomy and Physiology of the Basal Ganglia and Thalami
- •Selected References
- •Alcohol and Related Disorders
- •Opioids and Derivatives
- •Inhaled Gases and Toxins
- •Selected References
- •Selected References
- •Hypertensive Encephalopathies
- •Glucose Disorders
- •Thyroid Disorders
- •Seizures and Related Disorders
- •Miscellaneous Disorders
- •Selected References
- •The Normal Aging Brain
- •Dementias
- •Degenerative Disorders
- •Selected References
- •Normal Variants
- •Hydrocephalus
- •CSF Leaks and Sequelae
- •Selected References
- •Cerebral Hemisphere Formation
- •Imaging Approach to Brain Malformations
- •Posterior Fossa Anatomy
- •Chiari Malformations
- •Hindbrain Malformations
- •Selected References
- •Commissural Anomalies
- •Malformations Secondary to Abnormal Postmigrational Development
- •Selected References
- •Anencephaly
- •Holoprosencephaly
- •Holoprosencephaly Variants
- •Related Midline Disorders
- •Holoprosencephaly Mimics
- •Selected References
- •Selected References
- •Selected References
- •Cephaloceles
- •Craniosynostoses
- •Meningeal Anomalies
- •Selected References
- •Index

Nonneoplastic Tumor-Associated
Cysts
Terminology
Tumor-associated cysts (TACs) are benign cysts that are adjacent to, but not contained within, a neoplasm.
TACs are also referred to as peritumoral cysts. Surgeons sometimes call them "herald" cysts, as they are immediately adjacent to (and thus "herald" the presence of) a tumor mass.
Etiology
Whether TACs are true arachnoid cysts or fluid collections mostly lined by compressed gliotic brain is debatable. Cyst formation may also relate to blood-brain-barrier deficiency with peritumoral extravasation of water, electrolytes, and plasma proteins from altered microvessels.
TACs are usually associated with benign extraaxial tumors, such as meningioma, schwannoma, pituitary macroadenoma, and craniopharyngioma. TACs are found in both supraand infratentorial compartments.
Pathology
Most TACs represent trapped, encysted "pools" of CSF adjacent to a large extraaxial neoplasm (28-29). The contents of these peritumoral collections vary from clear CSF-like liquid to turbid proteinaceous fluid. The cyst wall generally consists of gliotic brain with reactive astrocytes and lymphocytes. No tumor cells are present.
Location. TACs are usually positioned at the tumor-brain interface between the mass and adjacent cortex.
Size and Number. TACs vary from small insignificant collections to very large cysts. Most are solitary, but occasionally multiple loculated fluid collections are trapped at the tumor-brain interface.
Clinical Issues
Unless a TAC becomes unusually large, symptoms are generally related to the neoplasm itself, not the TAC.
Imaging
General Features. The common appearance is one or more "pools" of trapped fluid surrounding an extraaxial tumor mass
(28-30).
CT Findings. TACs are hypodense to brain and usually isoto slightly hyperdense compared with CSF. No calcification, hemorrhage, or enhancement is present.
MR Findings. Signal intensity varies with protein content. Most TACs are hypointense to brain on T1WI and very hyperintense on PD and T2WI (28-32). Hemorrhage with blood-fluid levels may be present (28-31) (28-32). Suppression on FLAIR is variable. Enhancement is minimal or absent and generally related to reactive inflammatory changes in the cyst wall, not tumor.
Nonneoplastic Cysts
887
Differential Diagnosis
TACs must be distinguished from cystic neoplasms, arachnoid cyst (not tumor-associated), and enlarged perivascular (Virchow-Robin) spaces (see below). The latter two behave like CSF on imaging studies.
Parenchymal Cysts
Parenchymal (intraaxial) cysts are much more common than either their extraaxial or intraventricular counterparts. Once a cyst has been identified as lying within the brain itself, the differential diagnosis is limited. The most common parenchymal cysts—prominent perivascular spaces and hippocampal sulcus remnants—are anatomic variants. Neuroglial cysts and porencephalic cysts are relatively uncommon. All other nonneoplastic, noninfectious brain cysts are rare.
Enlarged Perivascular Spaces
By far the most common parenchymal brain "cysts" are enlarged perivascular spaces (PVSs). They vary from solitary, small, inconspicuous, and unremarkable to multiple, large, bizarre, alarming-looking collections of CSF-like fluid. They are often asymmetric, may cause mass effect, and have frequently been mistaken for multicystic brain tumors.
Terminology
PVSs are also known as Virchow-Robin spaces. PVSs are pialined spaces that accompany penetrating arteries and arterioles into the brain parenchyma. The PVSs do not communicate directly with the subarachnoid space.
Etiology
General Concepts. The brain PVSs form a complicated intraparenchymal network that is distributed throughout the cerebral hemispheres, midbrain, and cerebellum. They are filled with interstitial fluid (ISF), not CSF, and are thought to be a major pathway for ISF and cerebral metabolites to exit the brain. Recent evidence suggests the PVSs also perform an essential role in maintaining intracranial pressure homeostasis.
Precisely why some PVSs become enlarged is unknown. Most investigators believe ISF egress is blocked, causing cystic enlargement of the PVSs.
Genetics. Sporadic PVS enlargement has no known genetic predilection. Patients with Hurler, Hunter, or Sanfilippo disease accumulate undegraded mucopolysaccharides within enlarged PVSs. A few congenital muscular dystrophies have also been associated with cystic PVSs.
Pathology
Location. Although PVSs can be found virtually anywhere in the brain, they have a striking predilection for the inferior third of the basal ganglia, especially near the anterior commissure
Neoplasms, Cysts, and Tumor-Like Lesions
888
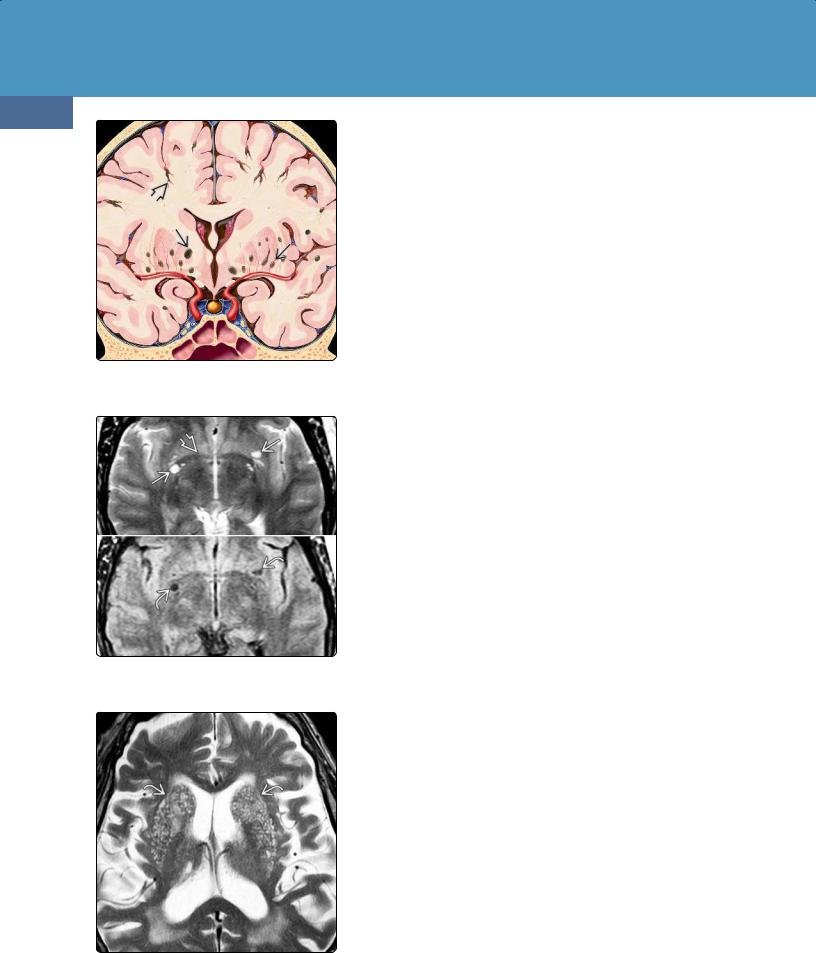
(28-33) Graphic shows normal PVSs along penetrating arteries in the basal ganglia and subcortical white matter .
(28-34) (Top) T2WI shows perivascular spaces clustered around the anterior commissure . ISF-filled VRSs suppress on FLAIR (bottom).
(28-35) Basal ganglia PVSs can become very prominent in older patients , a condition termed "état criblé" or cribriform state.
(28-33). They are also common in the subcortical and deep white matter as well as the midbrain and dentate nuclei of the cerebellum.
Size and Number. Enlarged PVSs tend to occur in clusters. Collections of multiple variably sized PVSs are much more common than solitary unilocular lesions.
Most PVSs are smaller than 2 mm. PVSs increase in size and prevalence with age (28-35). Giant so-called tumefactive PVSs measuring up to 9 cm in diameter have been reported.
Gross Pathology. Enlarged PVSs appear as collections of smoothly demarcated cysts filled with clear colorless fluid (28-36).
Microscopic Features. PVSs are bounded by a single or double layer of invaginated pia. Cortical PVSs are lined by a single layer of pia, whereas two layers accompany lenticulostriate and midbrain arteries.
As a PVS penetrates into the subcortical white matter, it becomes fenestrated and discontinuous. The pial layer disappears completely at the capillary level.
The brain parenchyma surrounding enlarged PVSs is typically normal without gliosis, inflammation, hemorrhage, or discernible amyloid deposition.
Clinical Issues
Epidemiology. PVSs are the most common nonneoplastic parenchymal brain "cysts." With high-resolution 3.0-T MR, small PVSs are seen in nearly all patients (28-34), in virtually every location, and at all ages. Between 25-30% of children have identifiable PVSs on high-resolution MR scans.
Demographics. Enlarged PVSs are more common in middle-aged and older patients and increase in both size and number with age (28-35). Recent studies have linked enlarged PVSs with age, lacunar stroke subtype, and white matter lesions and consider them as an MR marker of cerebral small vessel disease.
Presentation. Most enlarged PVSs do not cause symptoms and are discovered incidentally on imaging studies or at autopsy. Neuropsychological evaluation is typically normal. Nonspecific symptoms such as headache, dizziness, memory impairment, and Parkinson-like symptoms have been reported in some cases, but their relationship to enlarged PVSs is unclear. Large PVSs in the midbrain may cause obstructive hydrocephalus and present with headache.
Natural History. Enlarged PVSs tend to be stable in size and remain unchanged over many years although a few cases of progressively enlarging PVSs have been reported.
Treatment Options. Enlarged PVSs are "leave me alone" lesions that should not be mistaken for serious disease. If midbrain PVSs cause obstructive hydrocephalus, the generally accepted treatment is to shunt the ventricles, not the cysts.
Imaging
General Features. The common pattern of enlarged PVSs is one or more clusters of variably sized CSF-like cysts. They commonly cause focal mass effect. For example, if they occur in the subcortical white matter, the overlying gyri are enlarged with concomitant compression of adjacent sulci
(28-38).
CT Findings. Enlarged PVSs are groups of round/ovoid/linear/punctate CSF-like lesions that do not demonstrate calcification or hemorrhage (28-37). PVSs do not enhance following contrast administration.
MR Findings. Even though they are filled with ISF, PVSs closely parallel CSF signal intensity on all imaging sequences. Focal mass effect is common. Enlarged PVSs in the subcortical white matter expand overlying gyri (28-38) (28-39). Enlarged PVSs in the midbrain may compress the aqueduct and third ventricle, resulting in intraventricular obstructive hydrocephalus (28-36).
PVSs are isointense with CSF on T1-, PD, and T2WI. They suppress completely on FLAIR (28-34). Edema in the adjacent brain is absent although 25% of "tumefactive" PVSs have minimal increased signal intensity around the cysts.
PVSs do not hemorrhage, enhance, or demonstrate restricted diffusion.
Nonneoplastic Cysts
889
Differential Diagnosis
The major differential diagnosis is chronic lacunar infarction. Although they often affect the basal ganglia and suppress on FLAIR, lacunar infarcts do not cluster around the anterior commissure, are often irregular in shape, and frequently exhibit hyperintensity in the adjacent brain.
In some older patients, very prominent PVSs in the basal ganglia are present. This condition, called "état criblé" (cribriform state), should not be mistaken for multiple lacunar infarcts. PVSs are round/ovoid and regular in configuration, and the adjacent brain parenchymal is usually normal without gliosis or edema.
Infectious cysts (especially parenchymal neurocysticercosis cysts) are usually small. Although often multiple or multilocular, they typically do not occur in clusters of variably sized cysts as is typical for enlarged PVSs.
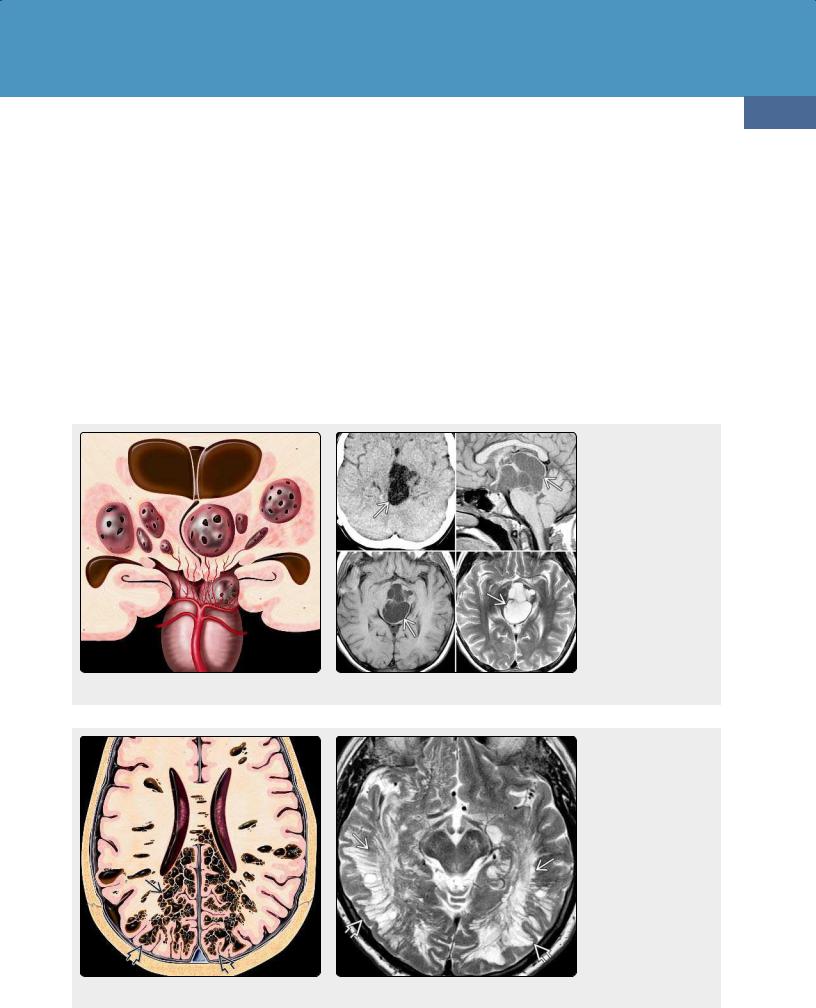
(28-36) Coronal graphic shows enlarged perivascular spaces in the midbrain and thalami that cause mass effect on the third ventricle and aqueduct with resulting hydrocephalus. (28-37) NECT and MR scans show a cluster of variably sized CSF-like cysts grossly expanding the midbrain. These are giant "tumefactive" perivascular spaces.
(28-38) Graphic depicts innumerable hemispheric enlarged PVSs in subcortical, deep white matter. Note that the overlying gyri are expanded but otherwise normal. (28-39) Axial T2WI in a 69y moderately demented man shows innumerable enlarged PVSs . Note sparing of overlying cortex, which appears expanded . (Courtesy M. WarmuthMetz, MD.)

Neoplasms, Cysts, and Tumor-Like Lesions
890
(28-40) Graphic of normal temporal lobe shows a string of cysts within the lateral hippocampus, along the residual cavity of the primitive hippocampal sulcus . Hippocampal sulcus remnant cysts are incidental, a normal finding.
ENLARGED PERIVASCULAR SPACES (PVSs)
Terminology
•Also known as Virchow-Robin spaces
•Found around penetrating blood vessels
•Lined by pia, filled with interstitial fluid
•Do not communicate directly with subarachnoid space
Pathology
•Normal PVSs common, < 2 cm
•Giant "tumefactive" PVSs up to 9 cm reported
•Basal ganglia, subcortical WM most common
Imaging
•Often bizarre-looking
•Occur in clusters
•Variably sized cysts
•Follow CSF
Hippocampal Sulcus Remnants
Terminology
Hippocampal sulcus remnants (HCSR) are also called hippocampal remnant cysts and hippocampal sulcal cavities.
Etiology
At 15 fetal weeks, the hippocampus normally unfolds and surrounds an "open" shallow fissure—the hippocampal sulcus—along the medial surface of the temporal lobe. The walls of the hippocampal sulcus gradually fuse, and the sulcus is eventually obliterated.
(28-41) Axial FLAIR scan shows hippocampal sulcus remnants as lines of tiny cysts medial to both temporal lobes. These contain CSF and therefore suppress completely on FLAIR.
At times, some segments of the closing hippocampal sulcus fail to fuse. One or more residual cystic cavities remain and persist into adult life. These remnant cavities—hippocampal remnant cysts—are normal anatomic variants (28-40).
Pathology
HCSRs are pia-lined cavities filled with CSF. Small blood vessels are often also included as the hippocampal sulcus forms, folds, and fuses.
Clinical Issues
HCSRs are incidental findings of no clinical significance. They do not cause seizures and are not related to trauma.
Imaging
HCSRs are seen in 10-15% of normal high-resolution MR scans. They appear as a "string of beads" with multiple small round or ovoid cysts curving along the hippocampus between the dentate gyrus and subiculum, just medial to the temporal horn of the lateral ventricle. HCSRs follow CSF in signal intensity on all sequences. They suppress completely on FLAIR (28-41), do not enhance, and do not restrict on DWI.
Differential Diagnosis
The major differential diagnosis HCSRs is enlarged perivascular spaces. When they occur in the temporal lobe, enlarged perivascular spaces are found in the subcortical white matter of the insula and anterior tip of the temporal lobe, not medial to the temporal horn of the lateral ventricle.
Neuroglial Cyst
Terminology
Neuroglial cysts (NGCs) are sometimes called glioependymal cysts or neuroepithelial cysts. They are benign fluid-containing cavities buried within the cerebral white matter.
Pathology
Location. Although NGCs occur throughout the neuraxis, they are usually supratentorial. The frontal lobe is the most common site. They often lie adjacent to—but do not communicate directly with—the cerebral ventricles.
Size and Number. Most NGCs are solitary unilocular cysts. They vary in size from a few millimeters up to several centimeters in diameter.
Gross Pathology. NGCs are rounded, smooth, unilocular cysts that contain clear CSF-like fluid.
Microscopic Features. Most NGCs are lined with a simple, nonstratified, low columnar/cuboidal epithelium (28-42). The epithelium usually sits directly on deep cerebral WM without an intervening capsule or basement membrane.
Clinical Issues
Epidemiology. Parenchymal NGCs are uncommon, representing less than 1% of all intracranial cysts.
Demographics. NGCs occur in all age groups but are generally more common in adults. There is no sex predilection.
Presentation. NGCs are often asymptomatic and found incidentally at imaging or autopsy. The most common presenting symptom, if any, is headache.
Natural History. Many—if not most—NGCs remain stable over many years.
Treatment Options. Serial observation with imaging studies is the usual course. Large NGCs have been fenestrated or drained.
Imaging
General Features. NGCs are smooth, round or ovoid, fluid-containing cysts.
CT Findings. NGCs are fluid density, typically resemble CSF, do not contain calcifications, and do not hemorrhage.
MR Findings. Signal intensity varies with cyst content. Most NGCs are isoor slightly hyperintense to CSF. They usually suppress on FLAIR, do not restrict, and do not enhance (28-43). The parenchyma surrounding an NGC is usually normal or may show minimal gliosis.
Differential Diagnosis
The diagnosis of NGC is mostly a process of elimination, excluding other, sometimes more ominous possibilities.
The major differential diagnosis of NGC is an enlarged perivascular space. Most enlarged PVSs are multiple (not solitary) and occur as clusters of variably sized cysts. A porencephalic cyst is a result of an insult to the brain parenchyma. Porencephalic cysts communicate with the ventricle and are lined by gliotic or spongiotic white matter.
Arachnoid cysts are extraaxial, not intraaxial, and are lined with flattened arachnoid cells. Epidermoid cysts are almost always extraaxial, do not
Nonneoplastic Cysts
891
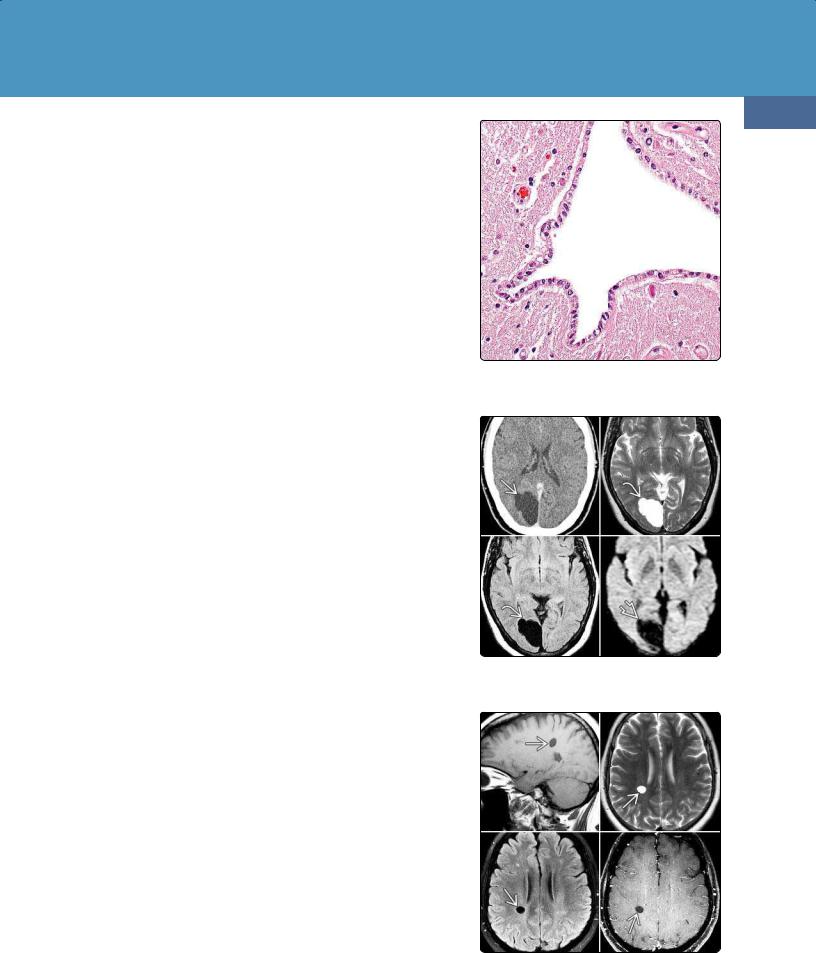
(28-42) Neuroglial cysts are lined by a single layer of cuboidal/low columnar epithelium. Cilia are rare. (Courtesy P. Burger, MD.)
(28-43) Proven neuroglial cyst in the right occipital lobe does not enhance on CECT , follows CSF on T2/FLAIR , does not restrict .
(28-44) MR shows a small presumed right parietal neuroglial cyst . The cyst follows CSF on all sequences and has been stable for 9 years.
Neoplasms, Cysts, and Tumor-Like Lesions
892
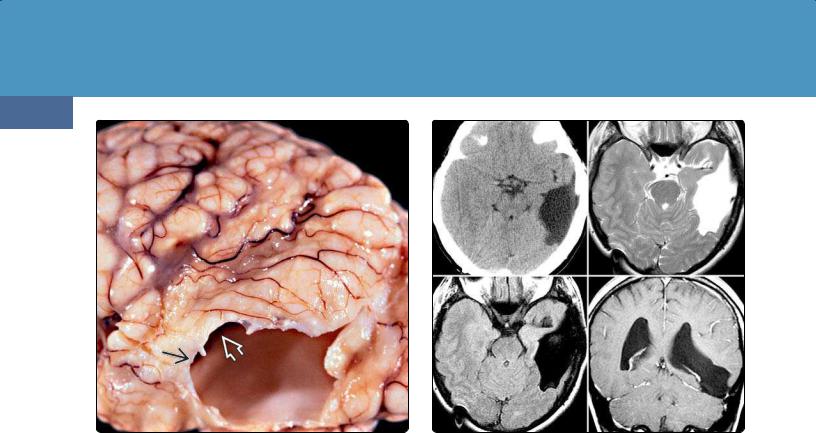
(28-45) Autopsy specimen shows a typical porencephalic cyst as a CSF-filled cavity that extends from the brain surface to the ventricular ependyma . (Courtesy J. Townsend, MD.)
(28-46) NECT, MR scans show a posttraumatic porencephalic cyst extending from the surface of the temporal lobe to the temporal horn of the lateral ventricle. The cyst contains CSF.
suppress on FLAIR, and restrict on DWI. Ependymal cysts are intraventricular.
Neoplastic and inflammatory cysts generally do not follow CSF, often demonstrate wall enhancement or calcification, and are frequently surrounded by edema.
A variety of miscellaneous periventricular cysts occur in newborns or children. Some may persist into adulthood. These include connatal cysts, germinolytic cysts, and cystic periventricular leukomalacia (PVL). Connatal cysts are cystic ependyma-lined areas adjacent to the superolateral margins of the body and frontal horns of the lateral ventricles. They are relatively common and generally innocuous lesions caused by coarctation or coaptation of the walls of the frontal horns.
Germinolytic cysts are glia-lined cysts that lie along the caudothalamic groove. They are associated with inherited metabolic disorders (e.g., Zellweger) and congenital infections (e.g., CMV), often contain septations or hemosiderin, and do not enhance. Cystic PVL most frequently occurs in premature infants and is located dorsolaterally to the bodies of the lateral ventricles.
Porencephalic Cyst
Terminology
"Porencephaly" literally means a hole in the brain. Porencephalic cysts are congenital or acquired CSF-filled parenchymal cavities that usually—but not invariably—communicate with the ventricular system. These cysts or cavities also often communicate via a "pore" with the subarachnoid space.
Etiology
Porencephalic cysts are encephaloclastic lesions, the end result of a destructive process (e.g., trauma, infection, vascular insult, surgery) that compromises brain parenchyma.
Most porencephalic cysts are sporadic. A few inherited syndromes (e.g., autosomal-dominant familial porencephaly) have been reported.
Pathology
Porencephalic cysts range in size from a few centimeters to cysts that involve virtually an entire cerebral hemisphere.
Porencephalic cysts are deep, unior bilateral, smooth-walled cavities or excavations within the brain parenchyma. They are often "full-thickness" lesions, extending from the ventricle to the glia limitans of the cortex (28-45). Occasionally, a thin rim of ependyma or subependymal white matter may separate the cyst from the ventricle.
Clinical Issues
Epidemiology. Porencephalic cysts are relatively common, especially in children, in whom they represent 2.5% of congenital brain lesions.
Presentation. Spastic hemiplegia, medically refractory epilepsy, and psychomotor retardation are the most common symptoms.
Natural History. Most porencephalic cysts remain stable for many years. Occasionally a porencephalic cyst will continue to sequester fluid and expand, causing mass effect.
