
- •Pineal Parenchymal Tumors
- •Germ Cell Tumors
- •Selected References
- •Medulloblastoma
- •Selected References
- •Anatomy of the Cranial Meninges
- •Meningomas
- •Primary Melanocytic Lesions
- •Other Related Neoplasms
- •Selected References
- •Cranial Nerve Anatomy
- •Schwannomas
- •Neurofibromas
- •Selected References
- •Histiocytic Tumors
- •Selected References
- •Sellar Region Anatomy
- •Normal Imaging Variants
- •Congenital Lesions
- •Neoplasms
- •Miscellaneous Lesions
- •Selected References
- •Intracranial Pseudotumors
- •Selected References
- •Metastatic Lesions
- •Paraneoplastic Syndromes
- •Selected References
- •Scalp Cysts
- •Extraaxial Cysts
- •Parenchymal Cysts
- •Intraventricular Cysts
- •Selected References
- •Anatomy and Physiology of the Basal Ganglia and Thalami
- •Selected References
- •Alcohol and Related Disorders
- •Opioids and Derivatives
- •Inhaled Gases and Toxins
- •Selected References
- •Selected References
- •Hypertensive Encephalopathies
- •Glucose Disorders
- •Thyroid Disorders
- •Seizures and Related Disorders
- •Miscellaneous Disorders
- •Selected References
- •The Normal Aging Brain
- •Dementias
- •Degenerative Disorders
- •Selected References
- •Normal Variants
- •Hydrocephalus
- •CSF Leaks and Sequelae
- •Selected References
- •Cerebral Hemisphere Formation
- •Imaging Approach to Brain Malformations
- •Posterior Fossa Anatomy
- •Chiari Malformations
- •Hindbrain Malformations
- •Selected References
- •Commissural Anomalies
- •Malformations Secondary to Abnormal Postmigrational Development
- •Selected References
- •Anencephaly
- •Holoprosencephaly
- •Holoprosencephaly Variants
- •Related Midline Disorders
- •Holoprosencephaly Mimics
- •Selected References
- •Selected References
- •Selected References
- •Cephaloceles
- •Craniosynostoses
- •Meningeal Anomalies
- •Selected References
- •Index
Commissural and Cortical Maldevelopment
Malformations Secondary to Abnormal Postmigrational Development
According to Barkovich et al., the third group of cortical malformations is secondary to abnormal postmigrational development and typically reflects infectious or ischemic insults. This group was formerly designated "abnormalities of cortical organization." It is currently divided into four subtypes of polymicrogyria (PMG) according to whether clefts (schizencephaly) are present and whether they occur as part of a recognized multiple malformation syndrome or an inherited metabolic disorder.
Polymicrogyria
Terminology and Etiology
The signature feature of PMG is an irregular cortex with numerous small convolutions and shallow or obliterated sulci. The appearance is that of tiny miniature gyri piled on top of other disorganized gyri (37-43).
Mutations in the tubulin genes are common. The phenotypic spectrum of TUBA1A mutations includes bilateral perisylvian PMG with dysmorphic basal ganglia, cerebellar vermis dysplasia, and pontine hypoplasia.
Encephaloclastic insults such as infection (e.g., TORCH, Zika virus infection), intrauterine vascular accident (e.g., middle cerebral artery occlusion), trauma, and metabolic disorders have also been implicated in the development of PMG.
Pathology
Location. Bilateral perisylvian PMG is the most common location (61% of cases). Generalized (13%), frontal (5%), and parasagittal parietooccipital (3%) sites are less common. Associated periventricular GM heterotopias are found in 11% of cases, and other anomalies such as schizencephaly are common.
Gross Pathology. The gross findings of PMG vary widely. PMG can involve a single gyrus or most of an entire cerebral hemisphere. It can be unior bilateral, symmetric or asymmetric, and focal or diffuse.
Part or all of the brain surface is covered by innumerable heaped up and fused tiny gyri, giving it a "lumpy-bumpy" appearance that has been likened to the look and feel of Morocco leather (37-44). Bilateral disease—especially in the perisylvian regions—is present in the majority of cases. Abnormal lateral ventricle configuration and dysmorphic basal ganglia are common in PMG-associated tubulinopathies (37-46).
Microscopic Features. Microscopically, the cortical ribbon appears thin and excessively folded. Two main histological types of PMG—unlayered and fourlayered forms—occur. In the unlayered form, a continuous molecular layer is present without any discernible laminar organization. In four-layered PMG, the cortex shows complex folding, fusion, and branching. A laminar structure composed of a molecular layer, outer neuronal layer, nerve fiber layer, and inner neuronal layer is present.
Clinical Issues
1219
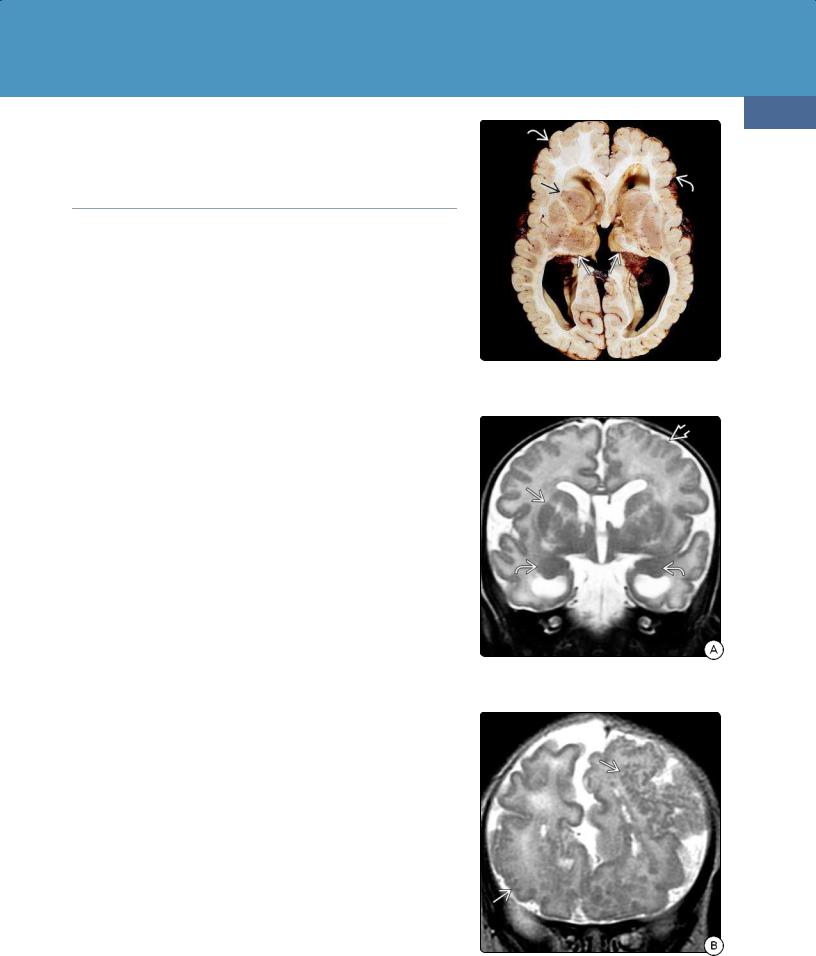
(37-46) Tubulinopathy shows PMG , grossly enlarged caudate heads , dysplastic-appearing putamina, small thalami . (R. Hewlett, MD.)
(37-47A) Coronal T2WI shows PMG with dysmorphic-appearing basal ganglia and large amygdalae .
PMG can present at any age. PMG is the most common imaging abnormality seen in infants with congenital cytomegalovirus infection. Some types of
(37-47B) More anterior coronal T2WI shows PMG as innumerable small nodular gray matter foci studding the surfaces of both hemispheres .

Congenital Malformations of the Skull and Brain
1220
PMG are more common in male patients, suggesting the involvement of X-linked genes.
Symptoms depend on the location and extent of PMG, ranging from global developmental delay to focal neurologic deficit(s) and seizures. Perisylvian PMG is a known congenital cause of bilateral opercular syndrome (Foix-Chauvany-Marie syndrome), which is characterized by paralysis of the facial, tongue, pharynx, and masticatory muscles.
Imaging
Multiplanar MR with high-resolution thin sections is required for complete delineation and detection of subtle lesions. Thickened or overfolded cortex with nodular surfaces and irregular "stippled" gray-white matter interfaces are the most characteristic findings (37-45). The basal ganglia often appear dysmorphic (37-47).
Diffusion-weighted imaging often demonstrates increased ADC values in the white matter underlying the PMG, the ipsilateral deep gray nuclei, and the corpus callosum.
Differential Diagnosis
The major differential diagnosis of polymicrogyria is type 2 lissencephaly (cobblestone malformation). The absence of congenital muscular dystrophy and "Z-shaped" brainstem is a helpful clinical distinction.
Sometimes pachygyria can be confused with PMG. The cortex in PMG is thin, nodular, and excessively folded. In focal cortical dysplasia, the gray matter is thickened, and the GMWM interface is blurred.
In schizencephaly, the dysplastic cortex lining the cleft may appear "pebbled," but the cleft distinguishes it from PMG.
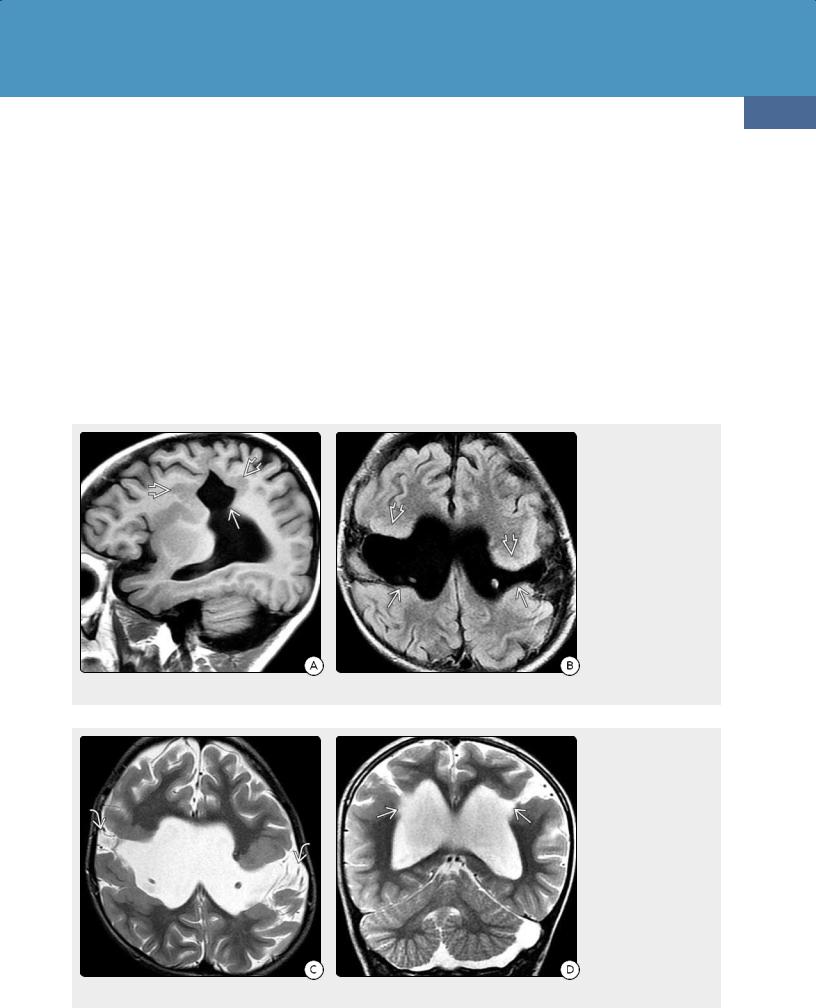
(37-48) Coronal oblique graphic shows an "open lip" schizencephaly in the frontal lobe. Note irregular gray-white matter interface of the cortex lining the cleft , indicating its dysplastic nature. (37-49) Autopsy shows bilateral schizencephalic clefts. Note that the thick, abnormal cortex curves over the "lips" of the clefts and follows them all the way medially to the ventricular ependyma. (Courtesy R. Hewlett, MD.)
(37-50A) NECT in a 19y man following minor head trauma shows the classic findings of unilateral schizencephaly. A nipplelike outpouching of CSF from the lateral ventricleis continuous with a thin "seam" of CSF that extends to the surface of the hemisphere. The cleft is lined with dysplastic-appearing GM. (37-50B) More cephalad scan shows cleftand dysplastic GM extending to ventricular ependyma .
Commissural and Cortical Maldevelopment
Schizencephaly
Terminology
Schizencephaly (literally meaning "split brain") is a gray-matter- lined cleft that extends from the ventricular ependyma to the pial surface of the cortex. The cleft spans the full thickness of the affected hemisphere (37-48).
Etiology
Once thought to represent an early malformation of cortical development, schizencephaly is now regarded as a disorder with heterogeneous causes. Destructive vascular lesions (e.g., middle cerebral artery occlusion) and infections (e.g., TORCH) occurring before 28 fetal weeks are considered likely etiologies. Focal destruction of radial glial fibers with impaired neuronal migration has been invoked as the potential consequence of these early vascular or infectious insults.
1221
COL4A1 mutation can cause schizencephaly and periventricular calcifications closely resembling congenital TORCH infection. COL4A1 encodes type IV collagen, which is expressed in all human tissues, especially the vasculature. Up to one-third of schizencephaly cases have an associated nonCNS abnormality secondary to vascular disruption (e.g., amniotic band syndrome or gastroschisis).
Pathology
Grossly, the brain exhibits a deep cleft that extends from its surface to the ventricle. The cleft is surrounded and lined by disorganized, dysmorphic-appearing cortex (37-49). The "lips" of the cleft can be fused or closely apposed ("closed lip" schizencephaly) or appear widely separated ("open lip" schizencephaly). Clefts may be associated with a range of other macroscopic abnormalities involving the septi pellucidi, corpus callosum, optic chiasm, and hippocampus.
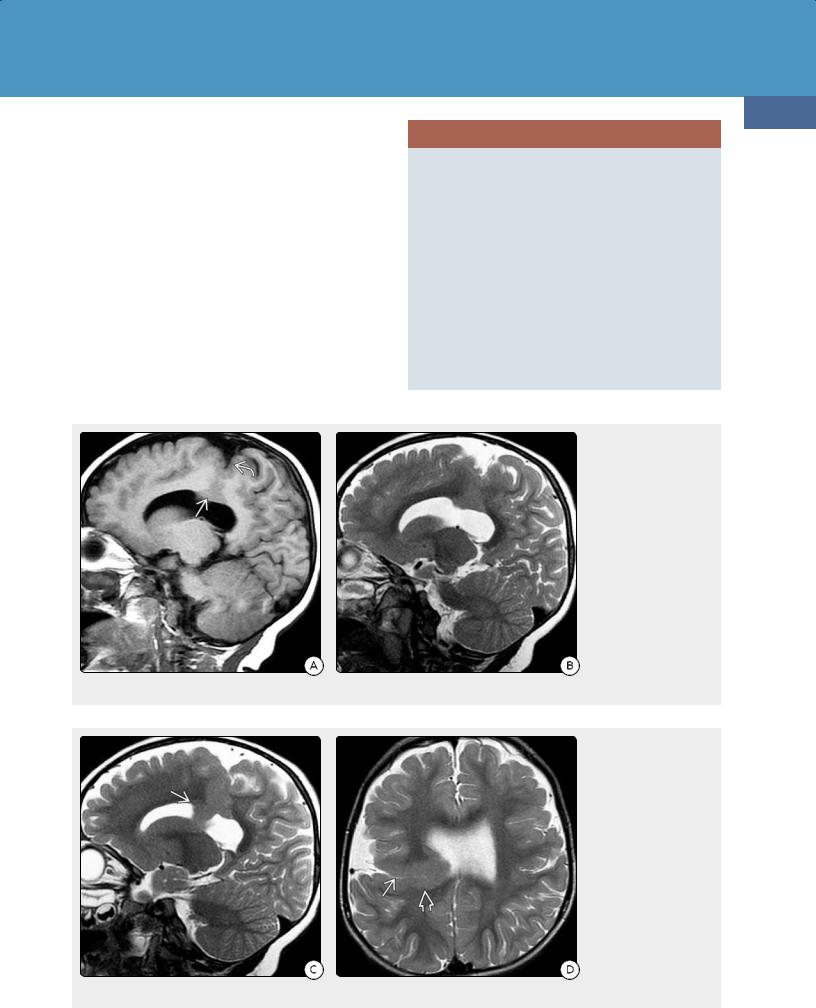
(37-51A) Sagittal T1WI shows a large CSF-filled cleft extending superiorly from the lateral ventricle. The cleft is lined with dysplasticappearing gray matter . (37-51B) FLAIR scan in the same patient shows bilateral schizencephalic clefts that are lined by dysplastic GM . The clefts suppress completely.
(37-51C) Axial T2WI shows that the open "lips" of both clefts contain prominent "flow voids" consistent with the primitive, "uncondensed" cortical veins that commonly accompany schizencephaly. (37-51D) Coronal T2WI shows the pointed "nipples" of CSF that extend outward from the ventricles into the schizencephalic clefts.

Congenital Malformations of the Skull and Brain
1222
Microscopically, the gray matter that lines the cleft is disorganized and does not exhibit normal cortical layers.
Clinical Issues
Schizencephaly is rare. There is no sex predilection. The most common clinical manifestations are drug-resistant epilepsy, developmental delay, and motor impairment. The severity of the motor and mental deficits correlates with the extent of the anatomic defect. "Open lip" clefts usually result in the most significant impairment. A unilateral "closed lip" cleft may cause only seizures. A few cases are discovered incidentally.
Imaging
The key imaging features of schizencephaly are (1) a CSF-filled defect extending from the ventricle wall to the pial surface and (2) dysplastic gray matter lining the cleft.
(37-52A) Axial T1WI shows severe "open lip" schizencephalic clefts in both hemispheres. (3752B) T2WI shows the thalami and some brain remnants in the frontal and occipital poles.
(37-52C) More cephalad scan shows presence of a falx and interhemispheric fissure distinguishing this extreme case of schizencephaly from holoprosencephaly. The remnant anterior, posterior "nubbins" of brain are different from the thin rim of cortex around the maximally enlarged lateral ventricles in severe hydrocephalus. (37-52D) Coronal T2WI shows no cortex external to the huge "open" schizencephalic clefts.
NECT scans typically show a focal V-shaped outpouching or "dimple" of CSF extending outward from the lateral ventricle (37-50). The clefts can be uni- (60%) or bilateral (40%) with prominent ("open lip") (37-52) or barely visible ("closed lip") (37-53). The cortex lining the cleft is hyperdense relative to white matter and interrupts the relatively uniform appearance of the corona radiata.
Common associated abnormalities are absent septi pellucidi (70% of cases) and a focally thinned or dysgenetic corpus callosum.
MR is more sensitive than CT, especially in delineating associated abnormalities, such as cortical dysplasia (polymicrogyria, pachygyria) and heterotopic gray matter. The cleft follows CSF signal intensity on all sequences (37-51) (3752) (37-53).
DSA or CTA/MRA have demonstrated occlusion or absence of the middle cerebral artery in some cases.
Commissural and Cortical Maldevelopment
Differential Diagnosis
The differential diagnosis of CSF-filled brain defects includes both developmental and destructive lesions. The major differential diagnosis of schizencephaly is porencephaly. In porencephaly, the cleft is lined by gliotic white matter, not dysplastic gray matter.
A large arachnoid cyst can mimic "open lip" schizencephaly. An arachnoid cyst displaces the adjacent cortex, which is otherwise normal in appearance. Occasionally, malformations in focal cortical development are seen with an arachnoid cyst.
Transmantle heterotopia or deeply infolded polymicrogyria may be difficult to distinguish from schizencephaly with closed, nearly fused "lips." Multiple imaging planes with highresolution T2WI or thin-section T1-weighted sequences with 3D reformatting and shaded surface displays are helpful in differentiating these entities.
1223
SCHIZENCEPHALY
Etiology
•In utero encephaloclastic lesion (vascular, infection)?
•COL4A1 mutation (can mimic TORCH)
Pathology
•Cleft ("seam") from ependyma to pia
○Can be closed or open, unior bilateral
○Lined by dysplastic gray matter
Imaging
•NECT
○Outpouching ("nipple") from lateral ventricle
○CSF-filled cleft lined with dysplastic GM
•MR
○Cleft lining follows cortex signal on all sequences
○Corpus callosum dysgenesis, other abnormalities common
(37-53A) Unilateral "closed lip" schizencephaly is illustrated by this case. Note gray matter extending from the ventricle to the pial surface of the brain . (37-53B) Sagittal T2WI shows that the GM lining the cleft is the same signal intensity as the cortex.
(37-53C) Sagittal T2WI shows that the heterotopic GM around the cleft bulges into the lateral ventricle body . (37-53D) Axial T2WI shows the heterotopic GMsurrounding the cleft, which is difficult to discern, as it is so thin.
