
- •Contents
- •Contributors
- •1 Introduction
- •2.1 Posterior Compartment
- •2.2 Anterior Compartment
- •2.3 Middle Compartment
- •2.4 Perineal Body
- •3 Compartments
- •3.1 Posterior Compartment
- •3.1.1 Connective Tissue Structures
- •3.1.2 Muscles
- •3.1.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2 Anterior Compartment
- •3.2.1 Connective Tissue Structures
- •3.2.2 Muscles
- •3.2.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2.4 Important Vessels, Nerves, and Lymphatics of the Anterior Compartment
- •3.3 Middle Compartment
- •3.3.1 Connective Tissue Structures
- •3.3.2 Muscles
- •3.3.3 Reinterpreted Anatomy and Clinical Relevance
- •3.3.4 Important Vessels, Nerves, and Lymphatics of the Middle Compartment
- •4 Perineal Body
- •References
- •MR and CT Techniques
- •1 Introduction
- •2.1 Introduction
- •2.2.1 Spasmolytic Medication
- •2.3.2 Diffusion-Weighted Imaging
- •2.3.3 Dynamic Contrast Enhancement
- •3 CT Technique
- •3.1 Introduction
- •3.2 Technical Disadvantages
- •3.4 Oral and Rectal Contrast
- •References
- •Uterus: Normal Findings
- •1 Introduction
- •References
- •1 Clinical Background
- •1.1 Epidemiology
- •1.2 Clinical Presentation
- •1.3 Embryology
- •1.4 Pathology
- •2 Imaging
- •2.1 Technique
- •2.2.1 Class I Anomalies: Dysgenesis
- •2.2.2 Class II Anomalies: Unicornuate Uterus
- •2.2.3 Class III Anomalies: Uterus Didelphys
- •2.2.4 Class IV Anomalies: Bicornuate Uterus
- •2.2.5 Class V Anomalies: Septate Uterus
- •2.2.6 Class VI Anomalies: Arcuate Uterus
- •2.2.7 Class VII Anomalies
- •References
- •Benign Uterine Lesions
- •1 Background
- •1.1 Uterine Leiomyomas
- •1.1.1 Epidemiology
- •1.1.2 Pathogenesis
- •1.1.3 Histopathology
- •1.1.4 Clinical Presentation
- •1.1.5 Therapy
- •1.1.5.1 Indications
- •1.1.5.2 Medical Therapy and Ablation
- •1.1.5.3 Surgical Therapy
- •1.1.5.4 Uterine Artery Embolization (UAE)
- •1.1.5.5 Magnetic Resonance-Guided Focused Ultrasound
- •2 Adenomyosis of the Uterus
- •2.1 Epidemiology
- •2.2 Pathogenesis
- •2.3 Histopathology
- •2.4 Clinical Presentation
- •2.5 Therapy
- •3 Imaging
- •3.2 Magnetic Resonance Imaging
- •3.2.1 Magnetic Resonance Imaging: Technique
- •3.2.2 MR Appearance of Uterine Leiomyomas
- •3.2.3 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.4 Histologic Subtypes and Forms of Degeneration
- •3.2.5 Differential Diagnosis
- •3.2.6 MR Appearance of Uterine Adenomyosis
- •3.2.7 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.8 Differential Diagnosis
- •3.3 Computed Tomography
- •3.3.1 CT Technique
- •3.3.2 CT Appearance of Uterine Leiomyoma and Adenomyosis
- •3.3.3 Atypical Appearances on CT and Differential Diagnosis
- •4.1 Indications
- •4.2 Technique
- •Bibliography
- •Cervical Cancer
- •1 Background
- •1.1 Epidemiology
- •1.2 Pathogenesis
- •1.3 Screening
- •1.4 HPV Vaccination
- •1.5 Clinical Presentation
- •1.6 Histopathology
- •1.7 Staging
- •1.8 Growth Patterns
- •1.9 Treatment
- •1.9.1 Treatment of Microinvasive Cervical Cancer
- •1.9.2 Treatment of Grossly Invasive Cervical Carcinoma (FIGO IB-IVA)
- •1.9.3 Treatment of Recurrent Disease
- •1.9.4 Treatment of Cervical Cancer During Pregnancy
- •1.10 Prognosis
- •2 Imaging
- •2.1 Indications
- •2.1.1 Role of CT and MRI
- •2.2 Imaging Technique
- •2.2.2 Dynamic MRI
- •2.2.3 Coil Technique
- •2.2.4 Vaginal Opacification
- •2.3 Staging
- •2.3.1 General MR Appearance
- •2.3.2 Rare Histologic Types
- •2.3.3 Tumor Size
- •2.3.4 Local Staging
- •2.3.4.1 Stage IA
- •2.3.4.2 Stage IB
- •2.3.4.3 Stage IIA
- •2.3.4.4 Stage IIB
- •2.3.4.5 Stage IIIA
- •2.3.4.6 Stage IIIB
- •2.3.4.7 Stage IVA
- •2.3.4.8 Stage IVB
- •2.3.5 Lymph Node Staging
- •2.3.6 Distant Metastases
- •2.4 Specific Diagnostic Queries
- •2.4.1 Preoperative Imaging
- •2.4.2 Imaging Before Radiotherapy
- •2.5 Follow-Up
- •2.5.1 Findings After Surgery
- •2.5.2 Findings After Chemotherapy
- •2.5.3 Findings After Radiotherapy
- •2.5.4 Recurrent Cervical Cancer
- •2.6.1 Ultrasound
- •2.7.1 Metastasis
- •2.7.2 Malignant Melanoma
- •2.7.3 Lymphoma
- •2.8 Benign Lesions of the Cervix
- •2.8.1 Nabothian Cyst
- •2.8.2 Leiomyoma
- •2.8.3 Polyps
- •2.8.4 Rare Benign Tumors
- •2.8.5 Cervicitis
- •2.8.6 Endometriosis
- •2.8.7 Ectopic Cervical Pregnancy
- •References
- •Endometrial Cancer
- •1.1 Epidemiology
- •1.2 Pathology and Risk Factors
- •1.3 Symptoms and Diagnosis
- •2 Endometrial Cancer Staging
- •2.1 MR Protocol for Staging Endometrial Carcinoma
- •2.2.1 Stage I Disease
- •2.2.2 Stage II Disease
- •2.2.3 Stage III Disease
- •2.2.4 Stage IV Disease
- •4 Therapeutic Approaches
- •4.1 Surgery
- •4.2 Adjuvant Treatment
- •4.3 Fertility-Sparing Treatment
- •5.1 Treatment of Recurrence
- •6 Prognosis
- •References
- •Uterine Sarcomas
- •1 Epidemiology
- •2 Pathology
- •2.1 Smooth Muscle Tumours
- •2.2 Endometrial Stromal Tumours
- •3 Clinical Background
- •4 Staging
- •5 Imaging
- •5.1 Leiomyosarcoma
- •5.2.3 Undifferentiated Uterine Sarcoma
- •5.3 Adenosarcoma
- •6 Prognosis and Treatment
- •References
- •1.1 Anatomical Relationships
- •1.4 Pelvic Fluid
- •2 Developmental Anomalies
- •2.1 Congenital Abnormalities
- •2.2 Ovarian Maldescent
- •3 Ovarian Transposition
- •References
- •1 Introduction
- •4 Benign Adnexal Lesions
- •4.1.1 Physiological Ovarian Cysts: Follicular and Corpus Luteum Cysts
- •4.1.1.1 Imaging Findings in Physiological Ovarian Cysts
- •4.1.1.2 Differential Diagnosis
- •4.1.2 Paraovarian Cysts
- •4.1.2.1 Imaging Findings
- •4.1.2.2 Differential Diagnosis
- •4.1.3 Peritoneal Inclusion Cysts
- •4.1.3.1 Imaging Findings
- •4.1.3.2 Differential Diagnosis
- •4.1.4 Theca Lutein Cysts
- •4.1.4.1 Imaging Findings
- •4.1.4.2 Differential Diagnosis
- •4.1.5 Polycystic Ovary Syndrome
- •4.1.5.1 Imaging Findings
- •4.1.5.2 Differential Diagnosis
- •4.2.1 Cystadenoma
- •4.2.1.1 Imaging Findings
- •4.2.1.2 Differential Diagnosis
- •4.2.2 Cystadenofibroma
- •4.2.2.1 Imaging Features
- •4.2.3 Mature Teratoma
- •4.2.3.1 Mature Cystic Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •4.2.3.2 Monodermal Teratoma
- •Imaging Findings
- •4.2.4 Benign Sex Cord-Stromal Tumors
- •4.2.4.1 Fibroma and Thecoma
- •Imaging Findings
- •4.2.4.2 Sclerosing Stromal Tumor
- •Imaging Findings
- •4.2.5 Brenner Tumors
- •4.2.5.1 Imaging Findings
- •4.2.5.2 Differential Diagnosis
- •5 Functioning Ovarian Tumors
- •References
- •1 Introduction
- •2.1 Context
- •2.2.2 Indications According to Simple Rules
- •References
- •CT and MRI in Ovarian Carcinoma
- •1 Introduction
- •2.1 Familial or Hereditary Ovarian Cancers
- •3 Screening for Ovarian Cancer
- •5 Tumor Markers
- •6 Clinical Presentation
- •7 Imaging of Ovarian Cancer
- •7.1.2 Peritoneal Carcinomatosis
- •7.1.3 Ascites
- •7.3 Staging of Ovarian Cancer
- •7.3.1 Staging by CT and MRI
- •Imaging Findings According to Tumor Stages
- •Value of Imaging
- •7.3.2 Prediction of Resectability
- •7.4 Tumor Types
- •7.4.1 Epithelial Ovarian Cancer
- •High-Grade Serous Ovarian Cancer
- •Low-Grade Serous Ovarian Cancer
- •Mucinous Epithelial Ovarian Cancer
- •Endometrioid Ovarian Carcinomas
- •Clear Cell Carcinomas
- •Imaging Findings of Epithelial Ovarian Cancers
- •Differential Diagnosis
- •Borderline Tumors
- •Imaging Findings
- •Differential Diagnosis
- •Recurrent Ovarian Cancer
- •Imaging Findings
- •Differential Diagnosis
- •Value of Imaging
- •Malignant Germ Cell Tumors
- •Dysgerminomas
- •Imaging Findings
- •Differential Diagnosis
- •Immature Teratomas
- •Imaging Findings
- •Malignant Transformation in Benign Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •Sex-Cord Stromal Tumors
- •Granulosa Cell Tumors
- •Imaging Findings
- •Sertoli-Leydig Cell Tumor
- •Imaging Findings
- •Ovarian Lymphoma
- •Imaging Findings
- •Differential Diagnosis
- •7.4.3 Ovarian Metastases
- •Imaging Findings
- •Differential Diagnosis
- •7.5 Fallopian Tube Cancer
- •7.5.1 Imaging Findings
- •Differential Diagnosis
- •References
- •Endometriosis
- •1 Introduction
- •2.1 Sonography
- •3 MR Imaging Findings
- •References
- •Vagina and Vulva
- •1 Introduction
- •3.1 CT Appearance
- •3.2 MRI Protocol
- •3.3 MRI Appearance
- •4.1 Imperforate Hymen
- •4.2 Congenital Vaginal Septa
- •4.3 Vaginal Agenesis
- •5.1 Vaginal Cysts
- •5.1.1 Gardner Duct Cyst (Mesonephric Cyst)
- •5.1.2 Bartholin Gland Cyst
- •5.2.1 Vaginal Infections
- •5.2.1.1 Vulvar Infections
- •5.2.1.2 Vulvar Thrombophlebitis
- •5.3 Vulvar Trauma
- •5.4 Vaginal Fistula
- •5.5 Post-Radiation Changes
- •5.6 Benign Tumors
- •6.1 Vaginal Malignancies
- •6.1.1 Primary Vaginal Carcinoma
- •6.1.1.1 MRI Findings
- •6.1.1.2 Lymph Node Drainage
- •6.1.1.3 Recurrence and Complications
- •6.1.2 Non-squamous Cell Carcinomas of the Vagina
- •6.1.2.1 Adenocarcinoma
- •6.1.2.2 Melanoma
- •6.1.2.3 Sarcomas
- •6.1.2.4 Lymphoma
- •6.2 Vulvar Malignancies
- •6.2.1 Vulvar Carcinoma
- •6.2.2 Melanoma
- •6.2.3 Lymphoma
- •6.2.4 Aggressive Angiomyxoma of the Vulva
- •7 Vaginal Cuff Disease
- •7.1 MRI Findings
- •8 Foreign Bodies
- •References
- •Imaging of Lymph Nodes
- •1 Background
- •3 Technique
- •3.1.1 Intravenous Unspecific Contrast Agents
- •3.1.2 Intravenous Tissue-Specific Contrast Agents
- •References
- •1 Introduction
- •2.1.1 Imaging Findings
- •2.1.2 Differential Diagnosis
- •2.1.3 Value of Imaging
- •2.2 Pelvic Inflammatory
- •2.2.1 Imaging Findings
- •2.3 Hydropyosalpinx
- •2.3.1 Imaging Findings
- •2.3.2 Differential Diagnosis
- •2.4 Tubo-ovarian Abscess
- •2.4.1 Imaging Findings
- •2.4.2 Differential Diagnosis
- •2.4.3 Value of Imaging
- •2.5 Ovarian Torsion
- •2.5.1 Imaging Findings
- •2.5.2 Differential Diagnosis
- •2.5.3 Diagnostic Value
- •2.6 Ectopic Pregnancy
- •2.6.1 Imaging Findings
- •2.6.2 Differential Diagnosis
- •2.6.3 Value of Imaging
- •3.1 Pelvic Congestion Syndrome
- •3.1.1 Imaging Findings
- •3.1.2 Differential Diagnosis
- •3.1.3 Value of Imaging
- •3.2 Ovarian Vein Thrombosis
- •3.2.1 Imaging Findings
- •3.2.2 Differential Diagnosis
- •3.2.3 Value of Imaging
- •3.3 Appendicitis
- •3.3.1 Imaging Findings
- •3.3.2 Value of Imaging
- •3.4 Diverticulitis
- •3.4.1 Imaging Findings
- •3.4.2 Differential Diagnosis
- •3.4.3 Value of Imaging
- •3.5 Epiploic Appendagitis
- •3.5.1 Imaging Findings
- •3.5.2 Differential Diagnosis
- •3.5.3 Value of Imaging
- •3.6 Crohn’s Disease
- •3.6.1 Imaging Findings
- •3.6.2 Differential Diagnosis
- •3.6.3 Value of Imaging
- •3.7 Rectus Sheath Hematoma
- •3.7.1 Imaging Findings
- •3.7.2 Differential Diagnosis
- •3.7.3 Value of Imaging
- •References
- •MRI of the Pelvic Floor
- •1 Introduction
- •2 Imaging Techniques
- •3.1 Indications
- •3.2 Patient Preparation
- •3.3 Patient Instruction
- •3.4 Patient Positioning
- •3.5 Organ Opacification
- •3.6 Sequence Protocols
- •4 MR Image Analysis
- •4.1 Bony Pelvis
- •5 Typical Findings
- •5.1 Anterior Compartment
- •5.2 Middle Compartment
- •5.3 Posterior Compartment
- •5.4 Levator Ani Muscle
- •References
- •Evaluation of Infertility
- •1 Introduction
- •2 Imaging Techniques
- •2.1 Hysterosalpingography
- •2.1.1 Cycle Considerations
- •2.1.2 Technical Considerations
- •2.1.3 Side Effects and Complications
- •2.1.5 Pathological Findings
- •2.1.6 Limitations of HSG
- •2.2.1 Cycle Considerations
- •2.2.2 Technical Considerations
- •2.2.2.1 Normal and Abnormal Anatomy
- •2.2.3 Accuracy
- •2.2.4 Side Effects and Complications
- •2.2.5 Limitations of Sono-HSG
- •2.3 Magnetic Resonance Imaging
- •2.3.1 Indications
- •2.3.2 Technical Considerations
- •2.3.3 Limitations
- •3 Ovulatory Dysfunction
- •4 Pituitary Adenoma
- •5 Polycystic Ovarian Syndrome
- •7 Uterine Disorders
- •7.1 Müllerian Duct Anomalies
- •7.1.1 Class I: Hypoplasia or Agenesis
- •7.1.2 Class II: Unicornuate
- •7.1.3 Class III: Didelphys
- •7.1.4 Class IV: Bicornuate
- •7.1.5 Class V: Septate
- •7.1.6 Class VI: Arcuate
- •7.1.7 Class VII: Diethylstilbestrol Related
- •7.2 Adenomyosis
- •7.3 Leiomyoma
- •7.4 Endometriosis
- •References
- •MR Pelvimetry
- •1 Clinical Background
- •1.3.1 Diagnosis
- •1.3.2.1 Cephalopelvic Disproportion
- •1.3.4 Inadequate Progression of Labor due to Inefficient Contraction (“the Powers”)
- •2.2 Palpation of the Pelvis
- •3 MR Pelvimetry
- •3.2 MR Imaging Protocol
- •3.3 Image Analysis
- •3.4 Reference Values for MR Pelvimetry
- •5 Indications for Pelvimetry
- •References
- •MR Imaging of the Placenta
- •2 Imaging of the Placenta
- •3 MRI Protocol
- •4 Normal Appearance
- •4.1 Placenta Variants
- •5 Placenta Adhesive Disorders
- •6 Placenta Abruption
- •7 Solid Placental Masses
- •9 Future Directions
- •References
- •Erratum to: Endometrial Cancer
298 |
R. Forstner |
|
|
to the pelvis and para-aortic lymph node were seen, whereas 13.5% was reported for pelvic resp for para-aortic lymph node metastases only (Bachmann et al. 2016).
Hematogenous spread occurs later in the course of the disease. Distant metastases are most commonly found in the liver, lung, pleura, and kidneys. At the time of the initial presentation, parenchymal liver metastases are extremely rare, and patients are more likely to present with liver surface metastases (Akin et al. 2008).
7.3\ Staging of Ovarian Cancer
Staging of ovarian cancer is determined by the extent and location of disease found at surgical staging. The latter is considered the gold standard for staging and aims for obtaining the histopathological diagnosis and a complete cytoreductive surgery. It includes a total abdominal hysterectomy, bilateral salpingo-oophorectomy, infracolic omentectomy, and lymphadenectomy (Jayson et al. 2014; Ozols et al. 2001). Furthermore, peritoneal cytology and multiple peritoneal biopsies are obtained throughout the pelvis and upper abdomen. In an attempt for optimal debulking, agressive surgery techniques including multidisciplinary surgery teams may be needed (Jayson et al. 2014). Laparoscopic staging procedures for ovarian cancer have also been introduced. In clinical practice, understaging of ovarian cancer remains a common problem (20–40%). This may occur when the initial surgery had been performed under the presumption of a benign tumor, due to laparoscopy technique, and lack of oncologic specialist expertise (Ozols et al. 2001).
Ovarian cancer is staged using the TNM or the FIGO (International Federation of Gynecology and Obstetrics) classification. According to the 2014 revised FIGO classification, not only the tumor stage but also the histological subtypes and grade should be documented. Most important change is the fusion of epithelial ovarian, fallopian, and primary peritoneal cancers. The revised staging classification is also used in germ cell and sex-cord stromal malignancies (Kandukuri and Rao 2015).
7.3.1\ Staging by CT and MRI
Surgical staging can be preceded by preoperative imaging. According to the ACR appropriateness criteria, radiographic studies such as contrast enema and urography have been replaced by CT and other cross-sectional imaging for staging ovarian cancer (Mitchell et al. 2013). Preoperative assessment by imaging has a major impact on treatment stratification, as the extent and anatomic location of peritoneal implants are major determinators for treatment decision (Forstner et al. 2010; Nougaret et al. 2012; Sala et al. 2013; Javadi et al. 2016).
Accurate mapping of the disease contributes to optimized surgery planning (Sala et al. 2013). This may also alert to need of multidisciplinary surgery teamwork. In case of extensive cancer load on CT or MRI, patients may also be triaged to undergo a neoadjuvant radiochemotherapy prior to surgery (Forstner et al. 2010; Sala et al. 2013).
Imaging Findings According to Tumor Stages
The FIGO classification system of ovarian cancer is summarized in Table 3.
Imaging findings in CT and MRI have also been adapted to the FIGO classification system (Forstner et al. 2010, 2016b; Nougaret et al. 2012; Javadi et al. 2016).
In stage I, tumor is confined to one ovary or the fallopian tube (stage IA) (Fig. 2) or both ovaries or the fallopian tubes (stage IB). The capsule of the tumor is intact, and there is no evidence of spread of the tumor outside of the ovary. In stage IC disease, tumor is detected on the ovarian or fallopian tube surface or capsule rupture has occurred. Malignant pelvic ascites may also be present (Fig. 1).
Stage II is characterized by local tumor extension into the pelvic soft tissues and to pelvic organs below the pelvic brim. In stage IIA, either direct tumor extension or implants on the uterus, ovaries, or fallopian tubes can be identified. Findings suggesting this stage include distortion or irregularity between the interface of the tumor and the myometrium. Stage IIB is characterized by involvement of pelvic tissues, such as the
CT and MRI in Ovarian Carcinoma |
299 |
|||||||||||||||||
|
|
|
|
|||||||||||||||
Table 3 FIGO classification of ovarian cancer |
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGO |
|
Subcategory and Findings |
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Stage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I |
A |
Tumor one ovary |
or fallopian tube |
|
|
|
|
|
|
|||||||
|
|
|
|
B |
Both ovaries |
fallopian tubes |
|
|
|
|
|
|
|
|||||
|
|
|
|
C |
One or both ovaries or fallopian tubes plus |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
C1: |
Surgical spill |
|
|
|
|
|
|
||||||
|
|
|
|
|
C2: Capsule ruptured or tumor on surface |
|
|
|
||||||||||
|
|
|
|
|
C3: M alignant cells in ascites or peritoneal washings |
|
||||||||||||
|
|
II |
A |
Extension/implants on uterus and/or ovaries and/or fallopian tubes |
|
|||||||||||||
|
|
|
|
B |
Extension to other pelvic intraperi toneal tissues |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
III |
A |
A1 |
Positive retroperitoneal LN only |
|
|
|
|
|
||||||||
|
|
|
|
|
A2 |
Microscopic extrapelvic peritoneal spread |
+/-LN |
|
|
|||||||||
|
|
|
|
B |
Peritoneal implants outside pelvis up to 2cm +/-LN |
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
C |
Peritoneal implants out side pelvis >2cm +/-LN |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
||||||||||
|
|
IV |
A |
|
Pleural effusion with positive cytology |
|
|
|
|
|||||||||
|
|
|
|
B |
Parenchymal metastasis, metastasis to extraperitoneal organs, |
|
||||||||||||
|
|
|
|
|
inguinal LN and LN outside abdominal cavity |
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Table modified from Kandukuri and Rao (2015) and Forstner et al. (2016b)
Changes in respect to the previous version are highlighted
LN lymph nodes
bladder, rectum, and pelvic peritoneum. Invasion of the sigmoid colon or rectum is diagnosed when loss of tissue plane between the solid components of the tumor, encasement, or localized wall thickening is noted (Fig. 10). A distance of less than 3 mm between the lesion and the pelvic sidewall or displacement or encasement of iliac vessels is suggestive of pelvic sidewall invasion (Fig. 11).
Stage III consists of extrapelvic peritoneal implants and/or retroperitoneal lymphadenopathy. Retroperitoneal lymph node metastases as the only disease outside the pelvis are found in less than 10%, but they demonstrate favorable prognosis than lymph node metastases in stages IIIB or IIIC (Kandukuri and Rao 2015). In imaging the diagnosis of lymphadenopathy is based on the short-axis diameter of lymph nodes of ≥1 cm. Peritoneal implants outside the pelvis, omental or mesenteric implants, and hepatic or splenic surface metastases are other findings defining stage
III ovarian cancer. Stages IIIA2–IIIC differ in the size of abdominal peritoneal lesions. In stage IIIA2, tumor is grossly limited to the pelvis; however, large amounts of ascites are a sign of upper abdominal peritoneal tumor spread. In stage IIIB, lesion size is 2 cm or less and in stage IIIC it exceeds 2 cm (Fig. 12). Ascites is a common finding in stage III disease. In delayed contrastenhanced MR imaging, ascites may enhance and thus obscure peritoneal implants.
Stage IV ovarian cancer is characterized by distant metastases that include pleura, parenchymal organs outside the pelvis, and extraabdominal lymph nodes. Malignant pleural effusion presents stage IVA1 and is characterized by pleural metastases proven either by positive cytology or biopsy. Typical imaging findings include pleural effusion associated with pleural nodularity and focal pleural thickening. Quantification of pleural effusion as small, moderate, or large has shown to be related with
300 |
R. Forstner |
|
|
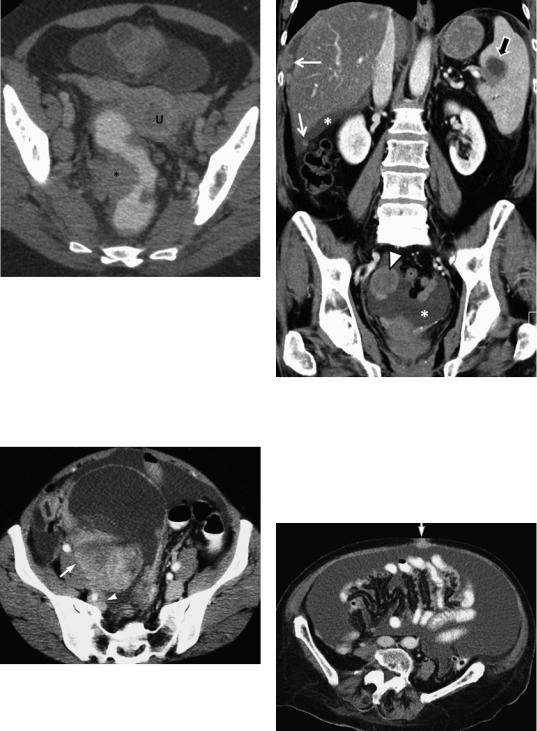
Fig. 10 Sigmoid colon wall invasion in CT. A peritoneal implant (*) shows a broad contact and impression of the colon wall. The ovarian cancer is located in the midline and compresses the bladder. Multiple pelvic lymph node metastases are seen, the largest in the right obturator region. U uterus
Fig. 11 Pelvic sidewall invasion. Transaxial CT at the level of the iliac bifurcation. A mixed solid and cystic adnexal tumor, which was nondifferentiated ovarian cancer at histopathology, is located in the pelvis. The left pelvic sidewall, including iliac vessels and psoas muscle, is clearly separated by fat. The right pelvic sidewall (arrow) is in direct contact with the solid tumor component. Furthermore, external and internal iliac arteries are displaced; the latter is encased by tumor (arrowhead)
Fig. 12 Stage IIIC ovarian cancer. Peritoneal nodular implants are shown at the diaphragm and in the Morison’s pouch (arrows). A surface metastases invading the spleen larger than 3 cm is also demonstrated (arrow). Ascites (*) is found in the pelvis and upper abdomen. Ovarian cancer (arrowhead)
Fig. 13 Ovarian cancer stage IVB. Large amounts of ascites indicate peritoneal metastases. Umbilical metastasis (arrow) is a finding typical of stage IVB ovarian cancer
