
- •Contents
- •Contributors
- •1 Introduction
- •2.1 Posterior Compartment
- •2.2 Anterior Compartment
- •2.3 Middle Compartment
- •2.4 Perineal Body
- •3 Compartments
- •3.1 Posterior Compartment
- •3.1.1 Connective Tissue Structures
- •3.1.2 Muscles
- •3.1.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2 Anterior Compartment
- •3.2.1 Connective Tissue Structures
- •3.2.2 Muscles
- •3.2.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2.4 Important Vessels, Nerves, and Lymphatics of the Anterior Compartment
- •3.3 Middle Compartment
- •3.3.1 Connective Tissue Structures
- •3.3.2 Muscles
- •3.3.3 Reinterpreted Anatomy and Clinical Relevance
- •3.3.4 Important Vessels, Nerves, and Lymphatics of the Middle Compartment
- •4 Perineal Body
- •References
- •MR and CT Techniques
- •1 Introduction
- •2.1 Introduction
- •2.2.1 Spasmolytic Medication
- •2.3.2 Diffusion-Weighted Imaging
- •2.3.3 Dynamic Contrast Enhancement
- •3 CT Technique
- •3.1 Introduction
- •3.2 Technical Disadvantages
- •3.4 Oral and Rectal Contrast
- •References
- •Uterus: Normal Findings
- •1 Introduction
- •References
- •1 Clinical Background
- •1.1 Epidemiology
- •1.2 Clinical Presentation
- •1.3 Embryology
- •1.4 Pathology
- •2 Imaging
- •2.1 Technique
- •2.2.1 Class I Anomalies: Dysgenesis
- •2.2.2 Class II Anomalies: Unicornuate Uterus
- •2.2.3 Class III Anomalies: Uterus Didelphys
- •2.2.4 Class IV Anomalies: Bicornuate Uterus
- •2.2.5 Class V Anomalies: Septate Uterus
- •2.2.6 Class VI Anomalies: Arcuate Uterus
- •2.2.7 Class VII Anomalies
- •References
- •Benign Uterine Lesions
- •1 Background
- •1.1 Uterine Leiomyomas
- •1.1.1 Epidemiology
- •1.1.2 Pathogenesis
- •1.1.3 Histopathology
- •1.1.4 Clinical Presentation
- •1.1.5 Therapy
- •1.1.5.1 Indications
- •1.1.5.2 Medical Therapy and Ablation
- •1.1.5.3 Surgical Therapy
- •1.1.5.4 Uterine Artery Embolization (UAE)
- •1.1.5.5 Magnetic Resonance-Guided Focused Ultrasound
- •2 Adenomyosis of the Uterus
- •2.1 Epidemiology
- •2.2 Pathogenesis
- •2.3 Histopathology
- •2.4 Clinical Presentation
- •2.5 Therapy
- •3 Imaging
- •3.2 Magnetic Resonance Imaging
- •3.2.1 Magnetic Resonance Imaging: Technique
- •3.2.2 MR Appearance of Uterine Leiomyomas
- •3.2.3 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.4 Histologic Subtypes and Forms of Degeneration
- •3.2.5 Differential Diagnosis
- •3.2.6 MR Appearance of Uterine Adenomyosis
- •3.2.7 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.8 Differential Diagnosis
- •3.3 Computed Tomography
- •3.3.1 CT Technique
- •3.3.2 CT Appearance of Uterine Leiomyoma and Adenomyosis
- •3.3.3 Atypical Appearances on CT and Differential Diagnosis
- •4.1 Indications
- •4.2 Technique
- •Bibliography
- •Cervical Cancer
- •1 Background
- •1.1 Epidemiology
- •1.2 Pathogenesis
- •1.3 Screening
- •1.4 HPV Vaccination
- •1.5 Clinical Presentation
- •1.6 Histopathology
- •1.7 Staging
- •1.8 Growth Patterns
- •1.9 Treatment
- •1.9.1 Treatment of Microinvasive Cervical Cancer
- •1.9.2 Treatment of Grossly Invasive Cervical Carcinoma (FIGO IB-IVA)
- •1.9.3 Treatment of Recurrent Disease
- •1.9.4 Treatment of Cervical Cancer During Pregnancy
- •1.10 Prognosis
- •2 Imaging
- •2.1 Indications
- •2.1.1 Role of CT and MRI
- •2.2 Imaging Technique
- •2.2.2 Dynamic MRI
- •2.2.3 Coil Technique
- •2.2.4 Vaginal Opacification
- •2.3 Staging
- •2.3.1 General MR Appearance
- •2.3.2 Rare Histologic Types
- •2.3.3 Tumor Size
- •2.3.4 Local Staging
- •2.3.4.1 Stage IA
- •2.3.4.2 Stage IB
- •2.3.4.3 Stage IIA
- •2.3.4.4 Stage IIB
- •2.3.4.5 Stage IIIA
- •2.3.4.6 Stage IIIB
- •2.3.4.7 Stage IVA
- •2.3.4.8 Stage IVB
- •2.3.5 Lymph Node Staging
- •2.3.6 Distant Metastases
- •2.4 Specific Diagnostic Queries
- •2.4.1 Preoperative Imaging
- •2.4.2 Imaging Before Radiotherapy
- •2.5 Follow-Up
- •2.5.1 Findings After Surgery
- •2.5.2 Findings After Chemotherapy
- •2.5.3 Findings After Radiotherapy
- •2.5.4 Recurrent Cervical Cancer
- •2.6.1 Ultrasound
- •2.7.1 Metastasis
- •2.7.2 Malignant Melanoma
- •2.7.3 Lymphoma
- •2.8 Benign Lesions of the Cervix
- •2.8.1 Nabothian Cyst
- •2.8.2 Leiomyoma
- •2.8.3 Polyps
- •2.8.4 Rare Benign Tumors
- •2.8.5 Cervicitis
- •2.8.6 Endometriosis
- •2.8.7 Ectopic Cervical Pregnancy
- •References
- •Endometrial Cancer
- •1.1 Epidemiology
- •1.2 Pathology and Risk Factors
- •1.3 Symptoms and Diagnosis
- •2 Endometrial Cancer Staging
- •2.1 MR Protocol for Staging Endometrial Carcinoma
- •2.2.1 Stage I Disease
- •2.2.2 Stage II Disease
- •2.2.3 Stage III Disease
- •2.2.4 Stage IV Disease
- •4 Therapeutic Approaches
- •4.1 Surgery
- •4.2 Adjuvant Treatment
- •4.3 Fertility-Sparing Treatment
- •5.1 Treatment of Recurrence
- •6 Prognosis
- •References
- •Uterine Sarcomas
- •1 Epidemiology
- •2 Pathology
- •2.1 Smooth Muscle Tumours
- •2.2 Endometrial Stromal Tumours
- •3 Clinical Background
- •4 Staging
- •5 Imaging
- •5.1 Leiomyosarcoma
- •5.2.3 Undifferentiated Uterine Sarcoma
- •5.3 Adenosarcoma
- •6 Prognosis and Treatment
- •References
- •1.1 Anatomical Relationships
- •1.4 Pelvic Fluid
- •2 Developmental Anomalies
- •2.1 Congenital Abnormalities
- •2.2 Ovarian Maldescent
- •3 Ovarian Transposition
- •References
- •1 Introduction
- •4 Benign Adnexal Lesions
- •4.1.1 Physiological Ovarian Cysts: Follicular and Corpus Luteum Cysts
- •4.1.1.1 Imaging Findings in Physiological Ovarian Cysts
- •4.1.1.2 Differential Diagnosis
- •4.1.2 Paraovarian Cysts
- •4.1.2.1 Imaging Findings
- •4.1.2.2 Differential Diagnosis
- •4.1.3 Peritoneal Inclusion Cysts
- •4.1.3.1 Imaging Findings
- •4.1.3.2 Differential Diagnosis
- •4.1.4 Theca Lutein Cysts
- •4.1.4.1 Imaging Findings
- •4.1.4.2 Differential Diagnosis
- •4.1.5 Polycystic Ovary Syndrome
- •4.1.5.1 Imaging Findings
- •4.1.5.2 Differential Diagnosis
- •4.2.1 Cystadenoma
- •4.2.1.1 Imaging Findings
- •4.2.1.2 Differential Diagnosis
- •4.2.2 Cystadenofibroma
- •4.2.2.1 Imaging Features
- •4.2.3 Mature Teratoma
- •4.2.3.1 Mature Cystic Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •4.2.3.2 Monodermal Teratoma
- •Imaging Findings
- •4.2.4 Benign Sex Cord-Stromal Tumors
- •4.2.4.1 Fibroma and Thecoma
- •Imaging Findings
- •4.2.4.2 Sclerosing Stromal Tumor
- •Imaging Findings
- •4.2.5 Brenner Tumors
- •4.2.5.1 Imaging Findings
- •4.2.5.2 Differential Diagnosis
- •5 Functioning Ovarian Tumors
- •References
- •1 Introduction
- •2.1 Context
- •2.2.2 Indications According to Simple Rules
- •References
- •CT and MRI in Ovarian Carcinoma
- •1 Introduction
- •2.1 Familial or Hereditary Ovarian Cancers
- •3 Screening for Ovarian Cancer
- •5 Tumor Markers
- •6 Clinical Presentation
- •7 Imaging of Ovarian Cancer
- •7.1.2 Peritoneal Carcinomatosis
- •7.1.3 Ascites
- •7.3 Staging of Ovarian Cancer
- •7.3.1 Staging by CT and MRI
- •Imaging Findings According to Tumor Stages
- •Value of Imaging
- •7.3.2 Prediction of Resectability
- •7.4 Tumor Types
- •7.4.1 Epithelial Ovarian Cancer
- •High-Grade Serous Ovarian Cancer
- •Low-Grade Serous Ovarian Cancer
- •Mucinous Epithelial Ovarian Cancer
- •Endometrioid Ovarian Carcinomas
- •Clear Cell Carcinomas
- •Imaging Findings of Epithelial Ovarian Cancers
- •Differential Diagnosis
- •Borderline Tumors
- •Imaging Findings
- •Differential Diagnosis
- •Recurrent Ovarian Cancer
- •Imaging Findings
- •Differential Diagnosis
- •Value of Imaging
- •Malignant Germ Cell Tumors
- •Dysgerminomas
- •Imaging Findings
- •Differential Diagnosis
- •Immature Teratomas
- •Imaging Findings
- •Malignant Transformation in Benign Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •Sex-Cord Stromal Tumors
- •Granulosa Cell Tumors
- •Imaging Findings
- •Sertoli-Leydig Cell Tumor
- •Imaging Findings
- •Ovarian Lymphoma
- •Imaging Findings
- •Differential Diagnosis
- •7.4.3 Ovarian Metastases
- •Imaging Findings
- •Differential Diagnosis
- •7.5 Fallopian Tube Cancer
- •7.5.1 Imaging Findings
- •Differential Diagnosis
- •References
- •Endometriosis
- •1 Introduction
- •2.1 Sonography
- •3 MR Imaging Findings
- •References
- •Vagina and Vulva
- •1 Introduction
- •3.1 CT Appearance
- •3.2 MRI Protocol
- •3.3 MRI Appearance
- •4.1 Imperforate Hymen
- •4.2 Congenital Vaginal Septa
- •4.3 Vaginal Agenesis
- •5.1 Vaginal Cysts
- •5.1.1 Gardner Duct Cyst (Mesonephric Cyst)
- •5.1.2 Bartholin Gland Cyst
- •5.2.1 Vaginal Infections
- •5.2.1.1 Vulvar Infections
- •5.2.1.2 Vulvar Thrombophlebitis
- •5.3 Vulvar Trauma
- •5.4 Vaginal Fistula
- •5.5 Post-Radiation Changes
- •5.6 Benign Tumors
- •6.1 Vaginal Malignancies
- •6.1.1 Primary Vaginal Carcinoma
- •6.1.1.1 MRI Findings
- •6.1.1.2 Lymph Node Drainage
- •6.1.1.3 Recurrence and Complications
- •6.1.2 Non-squamous Cell Carcinomas of the Vagina
- •6.1.2.1 Adenocarcinoma
- •6.1.2.2 Melanoma
- •6.1.2.3 Sarcomas
- •6.1.2.4 Lymphoma
- •6.2 Vulvar Malignancies
- •6.2.1 Vulvar Carcinoma
- •6.2.2 Melanoma
- •6.2.3 Lymphoma
- •6.2.4 Aggressive Angiomyxoma of the Vulva
- •7 Vaginal Cuff Disease
- •7.1 MRI Findings
- •8 Foreign Bodies
- •References
- •Imaging of Lymph Nodes
- •1 Background
- •3 Technique
- •3.1.1 Intravenous Unspecific Contrast Agents
- •3.1.2 Intravenous Tissue-Specific Contrast Agents
- •References
- •1 Introduction
- •2.1.1 Imaging Findings
- •2.1.2 Differential Diagnosis
- •2.1.3 Value of Imaging
- •2.2 Pelvic Inflammatory
- •2.2.1 Imaging Findings
- •2.3 Hydropyosalpinx
- •2.3.1 Imaging Findings
- •2.3.2 Differential Diagnosis
- •2.4 Tubo-ovarian Abscess
- •2.4.1 Imaging Findings
- •2.4.2 Differential Diagnosis
- •2.4.3 Value of Imaging
- •2.5 Ovarian Torsion
- •2.5.1 Imaging Findings
- •2.5.2 Differential Diagnosis
- •2.5.3 Diagnostic Value
- •2.6 Ectopic Pregnancy
- •2.6.1 Imaging Findings
- •2.6.2 Differential Diagnosis
- •2.6.3 Value of Imaging
- •3.1 Pelvic Congestion Syndrome
- •3.1.1 Imaging Findings
- •3.1.2 Differential Diagnosis
- •3.1.3 Value of Imaging
- •3.2 Ovarian Vein Thrombosis
- •3.2.1 Imaging Findings
- •3.2.2 Differential Diagnosis
- •3.2.3 Value of Imaging
- •3.3 Appendicitis
- •3.3.1 Imaging Findings
- •3.3.2 Value of Imaging
- •3.4 Diverticulitis
- •3.4.1 Imaging Findings
- •3.4.2 Differential Diagnosis
- •3.4.3 Value of Imaging
- •3.5 Epiploic Appendagitis
- •3.5.1 Imaging Findings
- •3.5.2 Differential Diagnosis
- •3.5.3 Value of Imaging
- •3.6 Crohn’s Disease
- •3.6.1 Imaging Findings
- •3.6.2 Differential Diagnosis
- •3.6.3 Value of Imaging
- •3.7 Rectus Sheath Hematoma
- •3.7.1 Imaging Findings
- •3.7.2 Differential Diagnosis
- •3.7.3 Value of Imaging
- •References
- •MRI of the Pelvic Floor
- •1 Introduction
- •2 Imaging Techniques
- •3.1 Indications
- •3.2 Patient Preparation
- •3.3 Patient Instruction
- •3.4 Patient Positioning
- •3.5 Organ Opacification
- •3.6 Sequence Protocols
- •4 MR Image Analysis
- •4.1 Bony Pelvis
- •5 Typical Findings
- •5.1 Anterior Compartment
- •5.2 Middle Compartment
- •5.3 Posterior Compartment
- •5.4 Levator Ani Muscle
- •References
- •Evaluation of Infertility
- •1 Introduction
- •2 Imaging Techniques
- •2.1 Hysterosalpingography
- •2.1.1 Cycle Considerations
- •2.1.2 Technical Considerations
- •2.1.3 Side Effects and Complications
- •2.1.5 Pathological Findings
- •2.1.6 Limitations of HSG
- •2.2.1 Cycle Considerations
- •2.2.2 Technical Considerations
- •2.2.2.1 Normal and Abnormal Anatomy
- •2.2.3 Accuracy
- •2.2.4 Side Effects and Complications
- •2.2.5 Limitations of Sono-HSG
- •2.3 Magnetic Resonance Imaging
- •2.3.1 Indications
- •2.3.2 Technical Considerations
- •2.3.3 Limitations
- •3 Ovulatory Dysfunction
- •4 Pituitary Adenoma
- •5 Polycystic Ovarian Syndrome
- •7 Uterine Disorders
- •7.1 Müllerian Duct Anomalies
- •7.1.1 Class I: Hypoplasia or Agenesis
- •7.1.2 Class II: Unicornuate
- •7.1.3 Class III: Didelphys
- •7.1.4 Class IV: Bicornuate
- •7.1.5 Class V: Septate
- •7.1.6 Class VI: Arcuate
- •7.1.7 Class VII: Diethylstilbestrol Related
- •7.2 Adenomyosis
- •7.3 Leiomyoma
- •7.4 Endometriosis
- •References
- •MR Pelvimetry
- •1 Clinical Background
- •1.3.1 Diagnosis
- •1.3.2.1 Cephalopelvic Disproportion
- •1.3.4 Inadequate Progression of Labor due to Inefficient Contraction (“the Powers”)
- •2.2 Palpation of the Pelvis
- •3 MR Pelvimetry
- •3.2 MR Imaging Protocol
- •3.3 Image Analysis
- •3.4 Reference Values for MR Pelvimetry
- •5 Indications for Pelvimetry
- •References
- •MR Imaging of the Placenta
- •2 Imaging of the Placenta
- •3 MRI Protocol
- •4 Normal Appearance
- •4.1 Placenta Variants
- •5 Placenta Adhesive Disorders
- •6 Placenta Abruption
- •7 Solid Placental Masses
- •9 Future Directions
- •References
- •Erratum to: Endometrial Cancer
MR Pelvimetry
Leonhard Schäffer, Ernst Beinder†,
and Rahel A. Kubik-Huch
Contents
1 Clinical Background\
1.1 Primary Versus Secondary
Cesarean Section\
1.2 Can Arrested Labor Be Treated
Effectively?\
1.3 Abnormal Length of Labor:
Diagnosis and Causes\
1.4 Interventional Management
of Inadequate Progression of Labor\
2 Clinical Methods of Pelvimetry\
2.1 External Pelvimetry and Evaluation
of Michaelis’s Rhomboid\
2.2 Palpation of the Pelvis\
3 MR Pelvimetry\
3.1 Safety Issues and Contraindications\ 3.2 MR Imaging Protocol\
3.3 Image Analysis\
3.4 Reference Values for MR Pelvimetry\
4 Can Pelvimetry Improve
Maternal and/or Fetal Outcome?\
5 Indications for Pelvimetry\
5.1 Breech Presentation and Maternal Preference for Spontaneous Delivery\
5.2 After Cesarean Section due to Arrest of Labor\
5.3 Clinically Conspicuous Abnormalities of Pelvic Shape and Status Post Pelvic Fracture\
References\
|
|
Abstract |
|
||
|
455 |
Arrest of labor with the necessity of perform- |
|||
ing secondary cesarean section is a major |
|||||
|
|
||||
|
456 |
cause of maternal morbidity and mortality. The |
|||
|
457 |
fetus is likewise affected by prolonged labor. |
|||
Pelvimetry is performed to identify those |
|||||
|
|
||||
|
457 |
women in whom an attempt at vaginal delivery |
|||
|
458 |
is likely to fail due to a narrow pelvis or pelvic |
|||
anomaly. Hence, the clinical significance of |
|||||
|
|
||||
458 |
pelvimetry depends on how the following |
||||
|
458 |
questions are answered: |
|||
•\ |
Is primary cesarean section associated with |
||||
|
459 |
||||
|
a lower morbidity and mortality of mother |
||||
|
459 |
|
|||
|
and child than secondary cesarean section |
||||
|
459 |
|
|||
|
after arrested labor has been diagnosed? |
||||
|
460 |
|
|||
•\ |
Can arrested labor be treated effectively? |
||||
|
460 |
||||
|
463 |
•\ |
Is there a reproducible method of pelvime- |
||
|
|
|
try with few side effects? |
||
|
463 |
•\ Is there evidence from randomized and |
|||
|
463 |
|
controlled studies that pelvimetry improves |
||
|
|
|
maternal and/or fetal outcome? |
||
463
464
1\ Clinical Background
464
464 Arrest of labor with the necessity of performing
secondary cesarean section is a major cause of maternal morbidity and mortality. The fetus is likewise affected by prolonged labor. Pelvimetry is performed to identify those women in whom an attempt at vaginal delivery is likely to fail due to a narrow pelvis or pelvic anomaly. Hence, the clinical significance of pelvimetry depends on how the following questions are answered:
Med Radiol Diagn Imaging (2017) |
455 |
DOI 10.1007/174_2017_2, © Springer International Publishing AG
Published Online: 11 February 2017
456 |
L. Schäffer et al. |
|
|
•\ Is primary cesarean section associated with a lower morbidity and mortality of mother and child than secondary cesarean section after arrested labor has been diagnosed?
•\ Can arrested labor be treated effectively?
•\ Is there a reproducible method of pelvimetry with few side effects?
•\ Is there evidence from randomized and controlled studies that pelvimetry improves maternal and/or fetal outcome?
1.1\ Primary Versus Secondary
Cesarean Section
The aim of pelvimetry is to identify maternal pelvic deviations that preclude vaginal delivery or would considerably prolong labor. If the results of pelvimetry suggest that vaginal delivery would be very difficult, primary cesarean section should be suggested. Both the mother and infant can thus be spared secondary cesarean section after protracted labor. The clinical significance of pelvimetry crucially depends on whether primary cesarean section can reduce maternal and fetal morbidity as compared with secondary cesarean section.
Cesarean section is performed as a primary (scheduled) or secondary (nonscheduled, after failure of labor to progress) procedure. The total number of cesarean sections, i.e., the sum of primary and secondary interventions, is 15–30% in Western industrialized countries. The mortality risk associated with vaginal delivery and cesarean section was determined in a study in Bavaria by Welsch (Müttersterblichkeit 2004).
Cesarean section mortality attributable to the intervention is defined as the number of deaths occurring per 1000 cesarean sections during or within 42 days of the intervention and that are due to surgical or anesthesia-related complications in women who were healthy before the operation and had no pregnancy-related risks. In the survey by Welsch, the maternal mortality risk of vaginal delivery versus cesarean section was 1:2.3 for the period from 1995 to 2000. However, the mortality rates no longer differ if only planned cesarean sections are compared with vaginal deliveries and may even be lower (D’Souza et al. 2013).
These figures underline that secondary cesarean sections after protracted labor or arrest of labor account for the excessive mortality of women during delivery.
Prolonged labor or arrest may have further adverse effects on mother and child:
•\ Perinatal morbidity and mortality: The duration of labor, in particular of the second stage, correlates with a decrease in fetal pH and pO2 and an increase in pCO2. Although fetal death during delivery has become rare, asphyxia contributes to perinatal morbidity. Detachment of the placenta due to uterine hyperactivity occurs in 1% of all pregnancies. Protracted labor often ends in vaginal operative delivery with the risk of fetal injury.
•\ Maternal morbidity: Protracted labor involves numerous complications for the mother. Rupture due to overextension of a uterus not operated on before is nearly always due to excessively prolonged labor. The higher need for vaginal operative delivery in women with protracted labor is associated with a higher rate of maternal injuries, pain, hematomas, urinary retention, and anemia as compared with spontaneous delivery (Angioli et al. 2000). Women with prolonged labor and secondary cesarean section have an increased risk of infection or puerperal fever. Atonic postpartum hemorrhage is a characteristic of long labor and again increases the risk of protracted recovery and infectious complications.
•\ Birth experience: No adequate systematic data are available on the emotional stress associated with prolonged and traumatic labor with secondary cesarean section. However, many women have problems coping with such an experience and do not become pregnant again. In summary, prolonged labor and secondary
cesarean section bear a considerable risk of maternal morbidity and mortality and also increase fetal morbidity. Modern obstetrical management therefore aims to ensure uncomplicated and speedy spontaneous delivery or, in women where this goal seems unattainable (or is not the mother’s preferred option), to plan elective primary cesarean section beforehand. Hence, techniques that can predict the probability of an uncomplicated vaginal delivery before the onset of labor are of the utmost clinical significance.
MR Pelvimetry |
457 |
|
|
1.2\ Can Arrested Labor Be Treated
Effectively?
Normal delivery is based on the complex interaction of maternal factors, fetal properties, and adequate labor. If this interaction of “passages, passenger, and powers” is disturbed, labor is protracted or even arrested. The failure of labor to progress is therefore not a diagnosis but a symptom that is amenable to treatment (e.g., when caused by inadequate uterine contractions) or not (e.g., absolute cephalopelvic disproportion). Isolated evaluation of either of the three factors, passages, passenger, and powers, is of limited value as, for instance, cephalopelvic disproportion can be diagnosed only if one looks at both the maternal pelvis and the fetus (“this pelvis is too small for this fetus”).
1.3\ Abnormal Length of Labor:
Diagnosis and Causes
1.3.1\ Diagnosis
The onset of delivery is most commonly defined as the occurrence of regular and painful uterine contractions that result in progressive dilatation and effacement of the cervix.
The course of delivery is determined by the following variables:
•\ Size and shape of the maternal pelvis
•\ Flexibility of the maternal soft tissues in the pelvis and adaptation of the ligaments and bony pelvis to the fetus
•\ Remodeling of the cervix
•\ Regular birth mechanism of the fetus
•\ Fetal head molding
•\ Efficient uterine contractions
The results reported by Friedman in the 1950s as the basis for diagnosing delayed labor have lately been updated (Zhang et al. 2010; Friedman 1955, 1956). Arrest of labor during the first stage (the stage of cervical dilatation) now is the absence of any progression of labor over a period of 4 h despite adequate contractions or 6 h with inadequate contractions diagnosed at cervical dilatation >6 cm and ruptured membranes corresponding to active phase of labor Spong et al. 2012).
The second stage (complete dilatation of the cervix until the onset of expulsive contractions) should not exceed 2 h of pushing in multiparous and 3 h of pushing in primiparous women. However, longer periods may be appropriate as long as progress is being documented and additional factors such as peridural anesthesia or malposition are present.
1.3.2\ Inadequate Progression
of Labor due to Maternal
Factors (“the Passage”)
1.3.2.1\ Cephalopelvic Disproportion
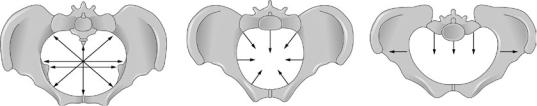
Failure of adequate progression of labor due to cephalopelvic disproportion with imminent fetal asphyxia is the most common reason to perform secondary cesarean section. Arrest is typically caused by a combination of a large infant, an abnormal birth mechanism, and a narrow maternal pelvis. Detectable abnormal narrowing with an absolute disproportion occurs in 0.5–1% of all deliveries today (Fig. 1). The incidence of
a |
b |
c |
Fig. 1 (a–c) Pelvic shapes from left to right: (a) normal pelvic shape and width (cranial view), (b) generally nar-
row pelvis (all pelvic parameters are shortened), (c) platypelloid pelvis with a markedly shorter obstetric conjugate

458 |
L. Schäffer et al. |
|
|
Table 1 Features of different pelvic shapes in comparison with the gynecoid (normal) pelvis
|
|
|
Obstetric |
Pelvic shape |
Pelvic inlet |
Pelvic outlet |
conjugate |
Android |
Normal |
Shorter |
Normal |
Anthropoid |
Shorter |
Normal |
Longer |
Platypelloid |
Longer |
Normal |
Shorter |
An android pelvis is associated with a higher incidence of deep transverse arrest, an anthropoid pelvis with a higher incidence of dorsoposterior position, and a platypelloid pelvis with high longitudinal position. All three pelvic shapes are characterized by protracted labor
borderline pelvic findings in which the size of the child and the birth mechanism together decide whether spontaneous delivery will be possible is much higher (Table 1).
Other maternal factors that may prolong or arrest labor include cervical leiomyomas or scarring of the cervix after prior surgery (conization, cerclage). Rare causes that prevent fetal descent are pelvic tumors such as large ovarian cysts or a pelvic kidney.
1.3.3\ Inadequate Progression
of Labor due to Fetal Factors (“the Passenger”)
An abnormal birth mechanism (malposition or malpresentation of the fetal head) prevents adequate progression of labor just as often as maternal factors. Other fetal causes are macrosomia or fetal anomalies associated with macrohydrocephalus or an abnormally large circumference of the fetal abdomen or rump (pronounced ascites, sacrococcygeal teratoma).
1.3.4\ Inadequate Progression of Labor due to Inefficient Contraction (“the Powers”)
Weak uterine contractions as a cause of inadequate progression of labor are most amenable to treatment. Inefficiency may become manifest as hypoactive, hyperactive, or uncoordinated contractions and hypertonic motility. Both hypoactivity and hyperactivity may occur secondary to mechanical obstruction.
1.4\ Interventional Management
of Inadequate Progression
of Labor
Of the three components involved in normal delivery (“passages, passenger, and powers”), only labor (“powers”) is easily amenable to treatment.
Assistance in women with hypoactive and uncoordinated contractions is recommended if progression is delayed and cephalopelvic disproportion has been excluded as the cause. Oxytocin is the drug of first choice (Cardozo et al. 1982).
In summary, arrested labor is often a multifactorial process resulting from the complex interaction of maternal pelvic size, size and presentation of the fetus, and labor activity. Effective therapeutic measures are only available for inadequate labor activity while no treatment is available for most other causes of arrested labor.
2\ Clinical Methods
of Pelvimetry
2.1\ External Pelvimetry
and Evaluation of Michaelis’s
Rhomboid
The normal values for the external pelvic measures are 25–26 cm for the interspinous distance, 28–29 cm for the intercrest distance, 31–32 cm for the intertrochanteric distance, and 20 cm for the external conjugate. The internal conjugate is calculated as the external conjugate minus 9 cm.
Michaelis’s rhomboid is the rectangular area over the sacral bone formed by the dimple below the spinal processes of L3 to L4 (upper depression), the two posterior spines of the ilia (lateral depressions), and the groove at the distal end of the vertebral column (lower depression). The rhomboid is usually a square, while its height increases considerably relative to its width in women with general narrowing of the pelvis. The lateral dimples are elevated in women with an android pelvis.
External pelvimetry will identify only pronounced deviations from the normal pelvic configuration that are rare in the European population.
