
- •Contents
- •Contributors
- •1 Introduction
- •2.1 Posterior Compartment
- •2.2 Anterior Compartment
- •2.3 Middle Compartment
- •2.4 Perineal Body
- •3 Compartments
- •3.1 Posterior Compartment
- •3.1.1 Connective Tissue Structures
- •3.1.2 Muscles
- •3.1.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2 Anterior Compartment
- •3.2.1 Connective Tissue Structures
- •3.2.2 Muscles
- •3.2.3 Reinterpreted Anatomy and Clinical Relevance
- •3.2.4 Important Vessels, Nerves, and Lymphatics of the Anterior Compartment
- •3.3 Middle Compartment
- •3.3.1 Connective Tissue Structures
- •3.3.2 Muscles
- •3.3.3 Reinterpreted Anatomy and Clinical Relevance
- •3.3.4 Important Vessels, Nerves, and Lymphatics of the Middle Compartment
- •4 Perineal Body
- •References
- •MR and CT Techniques
- •1 Introduction
- •2.1 Introduction
- •2.2.1 Spasmolytic Medication
- •2.3.2 Diffusion-Weighted Imaging
- •2.3.3 Dynamic Contrast Enhancement
- •3 CT Technique
- •3.1 Introduction
- •3.2 Technical Disadvantages
- •3.4 Oral and Rectal Contrast
- •References
- •Uterus: Normal Findings
- •1 Introduction
- •References
- •1 Clinical Background
- •1.1 Epidemiology
- •1.2 Clinical Presentation
- •1.3 Embryology
- •1.4 Pathology
- •2 Imaging
- •2.1 Technique
- •2.2.1 Class I Anomalies: Dysgenesis
- •2.2.2 Class II Anomalies: Unicornuate Uterus
- •2.2.3 Class III Anomalies: Uterus Didelphys
- •2.2.4 Class IV Anomalies: Bicornuate Uterus
- •2.2.5 Class V Anomalies: Septate Uterus
- •2.2.6 Class VI Anomalies: Arcuate Uterus
- •2.2.7 Class VII Anomalies
- •References
- •Benign Uterine Lesions
- •1 Background
- •1.1 Uterine Leiomyomas
- •1.1.1 Epidemiology
- •1.1.2 Pathogenesis
- •1.1.3 Histopathology
- •1.1.4 Clinical Presentation
- •1.1.5 Therapy
- •1.1.5.1 Indications
- •1.1.5.2 Medical Therapy and Ablation
- •1.1.5.3 Surgical Therapy
- •1.1.5.4 Uterine Artery Embolization (UAE)
- •1.1.5.5 Magnetic Resonance-Guided Focused Ultrasound
- •2 Adenomyosis of the Uterus
- •2.1 Epidemiology
- •2.2 Pathogenesis
- •2.3 Histopathology
- •2.4 Clinical Presentation
- •2.5 Therapy
- •3 Imaging
- •3.2 Magnetic Resonance Imaging
- •3.2.1 Magnetic Resonance Imaging: Technique
- •3.2.2 MR Appearance of Uterine Leiomyomas
- •3.2.3 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.4 Histologic Subtypes and Forms of Degeneration
- •3.2.5 Differential Diagnosis
- •3.2.6 MR Appearance of Uterine Adenomyosis
- •3.2.7 Locations, Growth Patterns, and Imaging Characteristics
- •3.2.8 Differential Diagnosis
- •3.3 Computed Tomography
- •3.3.1 CT Technique
- •3.3.2 CT Appearance of Uterine Leiomyoma and Adenomyosis
- •3.3.3 Atypical Appearances on CT and Differential Diagnosis
- •4.1 Indications
- •4.2 Technique
- •Bibliography
- •Cervical Cancer
- •1 Background
- •1.1 Epidemiology
- •1.2 Pathogenesis
- •1.3 Screening
- •1.4 HPV Vaccination
- •1.5 Clinical Presentation
- •1.6 Histopathology
- •1.7 Staging
- •1.8 Growth Patterns
- •1.9 Treatment
- •1.9.1 Treatment of Microinvasive Cervical Cancer
- •1.9.2 Treatment of Grossly Invasive Cervical Carcinoma (FIGO IB-IVA)
- •1.9.3 Treatment of Recurrent Disease
- •1.9.4 Treatment of Cervical Cancer During Pregnancy
- •1.10 Prognosis
- •2 Imaging
- •2.1 Indications
- •2.1.1 Role of CT and MRI
- •2.2 Imaging Technique
- •2.2.2 Dynamic MRI
- •2.2.3 Coil Technique
- •2.2.4 Vaginal Opacification
- •2.3 Staging
- •2.3.1 General MR Appearance
- •2.3.2 Rare Histologic Types
- •2.3.3 Tumor Size
- •2.3.4 Local Staging
- •2.3.4.1 Stage IA
- •2.3.4.2 Stage IB
- •2.3.4.3 Stage IIA
- •2.3.4.4 Stage IIB
- •2.3.4.5 Stage IIIA
- •2.3.4.6 Stage IIIB
- •2.3.4.7 Stage IVA
- •2.3.4.8 Stage IVB
- •2.3.5 Lymph Node Staging
- •2.3.6 Distant Metastases
- •2.4 Specific Diagnostic Queries
- •2.4.1 Preoperative Imaging
- •2.4.2 Imaging Before Radiotherapy
- •2.5 Follow-Up
- •2.5.1 Findings After Surgery
- •2.5.2 Findings After Chemotherapy
- •2.5.3 Findings After Radiotherapy
- •2.5.4 Recurrent Cervical Cancer
- •2.6.1 Ultrasound
- •2.7.1 Metastasis
- •2.7.2 Malignant Melanoma
- •2.7.3 Lymphoma
- •2.8 Benign Lesions of the Cervix
- •2.8.1 Nabothian Cyst
- •2.8.2 Leiomyoma
- •2.8.3 Polyps
- •2.8.4 Rare Benign Tumors
- •2.8.5 Cervicitis
- •2.8.6 Endometriosis
- •2.8.7 Ectopic Cervical Pregnancy
- •References
- •Endometrial Cancer
- •1.1 Epidemiology
- •1.2 Pathology and Risk Factors
- •1.3 Symptoms and Diagnosis
- •2 Endometrial Cancer Staging
- •2.1 MR Protocol for Staging Endometrial Carcinoma
- •2.2.1 Stage I Disease
- •2.2.2 Stage II Disease
- •2.2.3 Stage III Disease
- •2.2.4 Stage IV Disease
- •4 Therapeutic Approaches
- •4.1 Surgery
- •4.2 Adjuvant Treatment
- •4.3 Fertility-Sparing Treatment
- •5.1 Treatment of Recurrence
- •6 Prognosis
- •References
- •Uterine Sarcomas
- •1 Epidemiology
- •2 Pathology
- •2.1 Smooth Muscle Tumours
- •2.2 Endometrial Stromal Tumours
- •3 Clinical Background
- •4 Staging
- •5 Imaging
- •5.1 Leiomyosarcoma
- •5.2.3 Undifferentiated Uterine Sarcoma
- •5.3 Adenosarcoma
- •6 Prognosis and Treatment
- •References
- •1.1 Anatomical Relationships
- •1.4 Pelvic Fluid
- •2 Developmental Anomalies
- •2.1 Congenital Abnormalities
- •2.2 Ovarian Maldescent
- •3 Ovarian Transposition
- •References
- •1 Introduction
- •4 Benign Adnexal Lesions
- •4.1.1 Physiological Ovarian Cysts: Follicular and Corpus Luteum Cysts
- •4.1.1.1 Imaging Findings in Physiological Ovarian Cysts
- •4.1.1.2 Differential Diagnosis
- •4.1.2 Paraovarian Cysts
- •4.1.2.1 Imaging Findings
- •4.1.2.2 Differential Diagnosis
- •4.1.3 Peritoneal Inclusion Cysts
- •4.1.3.1 Imaging Findings
- •4.1.3.2 Differential Diagnosis
- •4.1.4 Theca Lutein Cysts
- •4.1.4.1 Imaging Findings
- •4.1.4.2 Differential Diagnosis
- •4.1.5 Polycystic Ovary Syndrome
- •4.1.5.1 Imaging Findings
- •4.1.5.2 Differential Diagnosis
- •4.2.1 Cystadenoma
- •4.2.1.1 Imaging Findings
- •4.2.1.2 Differential Diagnosis
- •4.2.2 Cystadenofibroma
- •4.2.2.1 Imaging Features
- •4.2.3 Mature Teratoma
- •4.2.3.1 Mature Cystic Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •4.2.3.2 Monodermal Teratoma
- •Imaging Findings
- •4.2.4 Benign Sex Cord-Stromal Tumors
- •4.2.4.1 Fibroma and Thecoma
- •Imaging Findings
- •4.2.4.2 Sclerosing Stromal Tumor
- •Imaging Findings
- •4.2.5 Brenner Tumors
- •4.2.5.1 Imaging Findings
- •4.2.5.2 Differential Diagnosis
- •5 Functioning Ovarian Tumors
- •References
- •1 Introduction
- •2.1 Context
- •2.2.2 Indications According to Simple Rules
- •References
- •CT and MRI in Ovarian Carcinoma
- •1 Introduction
- •2.1 Familial or Hereditary Ovarian Cancers
- •3 Screening for Ovarian Cancer
- •5 Tumor Markers
- •6 Clinical Presentation
- •7 Imaging of Ovarian Cancer
- •7.1.2 Peritoneal Carcinomatosis
- •7.1.3 Ascites
- •7.3 Staging of Ovarian Cancer
- •7.3.1 Staging by CT and MRI
- •Imaging Findings According to Tumor Stages
- •Value of Imaging
- •7.3.2 Prediction of Resectability
- •7.4 Tumor Types
- •7.4.1 Epithelial Ovarian Cancer
- •High-Grade Serous Ovarian Cancer
- •Low-Grade Serous Ovarian Cancer
- •Mucinous Epithelial Ovarian Cancer
- •Endometrioid Ovarian Carcinomas
- •Clear Cell Carcinomas
- •Imaging Findings of Epithelial Ovarian Cancers
- •Differential Diagnosis
- •Borderline Tumors
- •Imaging Findings
- •Differential Diagnosis
- •Recurrent Ovarian Cancer
- •Imaging Findings
- •Differential Diagnosis
- •Value of Imaging
- •Malignant Germ Cell Tumors
- •Dysgerminomas
- •Imaging Findings
- •Differential Diagnosis
- •Immature Teratomas
- •Imaging Findings
- •Malignant Transformation in Benign Teratoma
- •Imaging Findings
- •Differential Diagnosis
- •Sex-Cord Stromal Tumors
- •Granulosa Cell Tumors
- •Imaging Findings
- •Sertoli-Leydig Cell Tumor
- •Imaging Findings
- •Ovarian Lymphoma
- •Imaging Findings
- •Differential Diagnosis
- •7.4.3 Ovarian Metastases
- •Imaging Findings
- •Differential Diagnosis
- •7.5 Fallopian Tube Cancer
- •7.5.1 Imaging Findings
- •Differential Diagnosis
- •References
- •Endometriosis
- •1 Introduction
- •2.1 Sonography
- •3 MR Imaging Findings
- •References
- •Vagina and Vulva
- •1 Introduction
- •3.1 CT Appearance
- •3.2 MRI Protocol
- •3.3 MRI Appearance
- •4.1 Imperforate Hymen
- •4.2 Congenital Vaginal Septa
- •4.3 Vaginal Agenesis
- •5.1 Vaginal Cysts
- •5.1.1 Gardner Duct Cyst (Mesonephric Cyst)
- •5.1.2 Bartholin Gland Cyst
- •5.2.1 Vaginal Infections
- •5.2.1.1 Vulvar Infections
- •5.2.1.2 Vulvar Thrombophlebitis
- •5.3 Vulvar Trauma
- •5.4 Vaginal Fistula
- •5.5 Post-Radiation Changes
- •5.6 Benign Tumors
- •6.1 Vaginal Malignancies
- •6.1.1 Primary Vaginal Carcinoma
- •6.1.1.1 MRI Findings
- •6.1.1.2 Lymph Node Drainage
- •6.1.1.3 Recurrence and Complications
- •6.1.2 Non-squamous Cell Carcinomas of the Vagina
- •6.1.2.1 Adenocarcinoma
- •6.1.2.2 Melanoma
- •6.1.2.3 Sarcomas
- •6.1.2.4 Lymphoma
- •6.2 Vulvar Malignancies
- •6.2.1 Vulvar Carcinoma
- •6.2.2 Melanoma
- •6.2.3 Lymphoma
- •6.2.4 Aggressive Angiomyxoma of the Vulva
- •7 Vaginal Cuff Disease
- •7.1 MRI Findings
- •8 Foreign Bodies
- •References
- •Imaging of Lymph Nodes
- •1 Background
- •3 Technique
- •3.1.1 Intravenous Unspecific Contrast Agents
- •3.1.2 Intravenous Tissue-Specific Contrast Agents
- •References
- •1 Introduction
- •2.1.1 Imaging Findings
- •2.1.2 Differential Diagnosis
- •2.1.3 Value of Imaging
- •2.2 Pelvic Inflammatory
- •2.2.1 Imaging Findings
- •2.3 Hydropyosalpinx
- •2.3.1 Imaging Findings
- •2.3.2 Differential Diagnosis
- •2.4 Tubo-ovarian Abscess
- •2.4.1 Imaging Findings
- •2.4.2 Differential Diagnosis
- •2.4.3 Value of Imaging
- •2.5 Ovarian Torsion
- •2.5.1 Imaging Findings
- •2.5.2 Differential Diagnosis
- •2.5.3 Diagnostic Value
- •2.6 Ectopic Pregnancy
- •2.6.1 Imaging Findings
- •2.6.2 Differential Diagnosis
- •2.6.3 Value of Imaging
- •3.1 Pelvic Congestion Syndrome
- •3.1.1 Imaging Findings
- •3.1.2 Differential Diagnosis
- •3.1.3 Value of Imaging
- •3.2 Ovarian Vein Thrombosis
- •3.2.1 Imaging Findings
- •3.2.2 Differential Diagnosis
- •3.2.3 Value of Imaging
- •3.3 Appendicitis
- •3.3.1 Imaging Findings
- •3.3.2 Value of Imaging
- •3.4 Diverticulitis
- •3.4.1 Imaging Findings
- •3.4.2 Differential Diagnosis
- •3.4.3 Value of Imaging
- •3.5 Epiploic Appendagitis
- •3.5.1 Imaging Findings
- •3.5.2 Differential Diagnosis
- •3.5.3 Value of Imaging
- •3.6 Crohn’s Disease
- •3.6.1 Imaging Findings
- •3.6.2 Differential Diagnosis
- •3.6.3 Value of Imaging
- •3.7 Rectus Sheath Hematoma
- •3.7.1 Imaging Findings
- •3.7.2 Differential Diagnosis
- •3.7.3 Value of Imaging
- •References
- •MRI of the Pelvic Floor
- •1 Introduction
- •2 Imaging Techniques
- •3.1 Indications
- •3.2 Patient Preparation
- •3.3 Patient Instruction
- •3.4 Patient Positioning
- •3.5 Organ Opacification
- •3.6 Sequence Protocols
- •4 MR Image Analysis
- •4.1 Bony Pelvis
- •5 Typical Findings
- •5.1 Anterior Compartment
- •5.2 Middle Compartment
- •5.3 Posterior Compartment
- •5.4 Levator Ani Muscle
- •References
- •Evaluation of Infertility
- •1 Introduction
- •2 Imaging Techniques
- •2.1 Hysterosalpingography
- •2.1.1 Cycle Considerations
- •2.1.2 Technical Considerations
- •2.1.3 Side Effects and Complications
- •2.1.5 Pathological Findings
- •2.1.6 Limitations of HSG
- •2.2.1 Cycle Considerations
- •2.2.2 Technical Considerations
- •2.2.2.1 Normal and Abnormal Anatomy
- •2.2.3 Accuracy
- •2.2.4 Side Effects and Complications
- •2.2.5 Limitations of Sono-HSG
- •2.3 Magnetic Resonance Imaging
- •2.3.1 Indications
- •2.3.2 Technical Considerations
- •2.3.3 Limitations
- •3 Ovulatory Dysfunction
- •4 Pituitary Adenoma
- •5 Polycystic Ovarian Syndrome
- •7 Uterine Disorders
- •7.1 Müllerian Duct Anomalies
- •7.1.1 Class I: Hypoplasia or Agenesis
- •7.1.2 Class II: Unicornuate
- •7.1.3 Class III: Didelphys
- •7.1.4 Class IV: Bicornuate
- •7.1.5 Class V: Septate
- •7.1.6 Class VI: Arcuate
- •7.1.7 Class VII: Diethylstilbestrol Related
- •7.2 Adenomyosis
- •7.3 Leiomyoma
- •7.4 Endometriosis
- •References
- •MR Pelvimetry
- •1 Clinical Background
- •1.3.1 Diagnosis
- •1.3.2.1 Cephalopelvic Disproportion
- •1.3.4 Inadequate Progression of Labor due to Inefficient Contraction (“the Powers”)
- •2.2 Palpation of the Pelvis
- •3 MR Pelvimetry
- •3.2 MR Imaging Protocol
- •3.3 Image Analysis
- •3.4 Reference Values for MR Pelvimetry
- •5 Indications for Pelvimetry
- •References
- •MR Imaging of the Placenta
- •2 Imaging of the Placenta
- •3 MRI Protocol
- •4 Normal Appearance
- •4.1 Placenta Variants
- •5 Placenta Adhesive Disorders
- •6 Placenta Abruption
- •7 Solid Placental Masses
- •9 Future Directions
- •References
- •Erratum to: Endometrial Cancer

140 |
F. Collettini and B. Hamm |
|
|
which are histologically similar to carcinomas of the uterine corpus. They are of an intermediate to slightly high signal intensity on MRI and arise in the endocervix, from where they infiltrate the cervical stroma. In this type of tumor, it may be difficult to determine whether the origin is in the cervix or in the uterine corpus. In general, the part of the uterus from which the tumor arises shows deeper infiltration and more marked enlargement to the respective other part (cervix or corpus). The rare subtype of adenosquamous cervical carcinoma resembles squamous cell carcinoma with regard to its growth pattern and morphologic appearance on MR images.
Neuroendocrine cervical carcinoma is the second most frequent of the rare histologies. With its heterogeneous appearance and high signal intensity on T2-weighted images, neuroendocrine cervical carcinoma resembles squamous cell carcinoma at MRI (Lopes Dias et al. 2015).
2.3.3\ Tumor Size
Cervical cancer is revealed by MRI when tumors are large enough to be macroscopically visible, which is the case when the tumor has a diameter of 1–2 cm or a volume of 2–4 cm (Cancer Research UK 2016) (FIGO stage IB). Tumor size is the most important prognostic factor besides lymphatic metastasis. T2-weighted MRI in at least two planes is the method of first choice for determining tumor size (Hawighorst et al. 1997), since cervical cancer is best distinguished from surrounding tissue in these sequences. While gynecologic examination tends to underestimate tumor size with reported accuracy rates as low as 60%, MR imaging is very accurate in evaluating tumor size with 93% of cases within 5 mm of the histologic size (Hricak et al. 1988; Mitchell et al. 2006; Shiraiwa et al. 1999; Lopes Dias et al. 2015; Nicolet et al. 2000; Okamoto et al. 2003; Sahdev et al. 2007). Exact assessment of tumor size is crucial not only in patients with early-stage cervical cancer scheduled for fertility-sparing surgery, but also for patients with stage IIA cervical cancer or less, since patients with tumors larger than 4 cm are considered nonsurgical candidates. Preliminary comparative studies have shown that tumor delineation and determination of size
can be further enhanced by contrast medium administration. Preliminary comparative studies have shown that contrast-enhanced T1-weighted imaging may by superior to T2-weighted imaging in terms of cervical cancer localization and tumor margin detection, especially in patients with small tumors (Akita et al. 2011).
Tumor size is usually determined by measuring the longest diameter and its perpendicular. Two-dimensional measurement is based on the WHO guidelines for evaluating the response of solid tumors to chemotherapy or radiotherapy. Since a precise description of the spatial extent of a tumor is crucial prior to surgery, the tumor should also be measured in the third dimension. In patients where it is important to evaluate the response to radiochemotherapy, tumor size should be measured according to the revised RECIST1 (response evaluation criteria in solid tumors) guideline which uses one-dimensional measurements (Eisenhauer et al. 2009) (Fig. 13). These guidelines have superseded the twodimensional WHO measurement as the standard.
Techniques of tumor volumetry can additionally be applied. These techniques relied on formula such as height × width × length × π/6 to calculate approximate tumor volume or determined the volume by integration of the individual slice volumes (Fig. 12).
2.3.4\ Local Staging
2.3.4.1 Stage IA
There is no role for MR imaging in patients with microinvasive cervical cancer (stage IA). Microinvasive cervical cancers do not alter the normal morphologic MR appearance of the cervix (Fig. 15). The normal endocervix is depicted on T2-weighted images with a hyperintense, continuous mucosal layer surrounded by hypointense cervical stroma, consisting of connective tissue and smooth muscle. Hence, imaging is optional in patients with tumors IB1 or lower. Colposcopy and conization are the
1RECIST is a set of rules defining the criteria for tumoral response, stability, or progression during treatment. The longest diameter of the non-nodal lesions is measured.
Cervical Cancer |
141 |
|
|
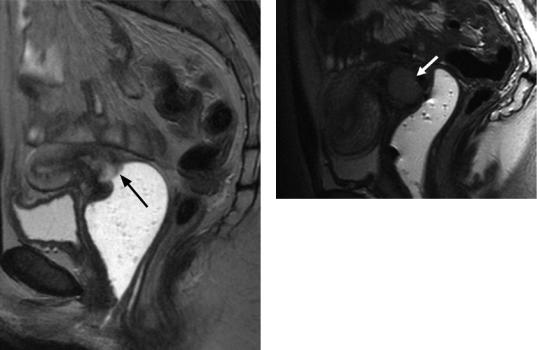
Fig.15 Stage IB. T2w TSE image in sagittal orientation. High-signal-intensity cervical cancer (arrow) primarily involving the anterior cervix and the portio. Gel filling of the vagina
methods of choice for evaluating these early forms of cervical carcinoma. The conization defect is depicted on MR images as a circumscribed lesion of the external os, quite often associated with an adjacent seroma or clot. In the further course, shrinkage of the portio can sometimes be seen.
2.3.4.2 Stage IB
Stage IB cervical carcinoma has a depth of more than 5 mm and a diameter of more than 7 mm or is visible clinically. The tumor is still confined to the cervix but is characterized by invasive local growth. This is the earliest stage that can be demonstrated by MRI (Mitchell et al. 2006). The average MRI detection rate is 95%. Stage IB1 (diameter <4 cm) and stage IB2 (diameter >4 cm) are distinguished based on their size. Stage IB2 cervical cancer has a poorer prognosis and should be treated with concomitant chemotherapy and radiation therapy. Transverse and sagittal T2-weighted images depict cervi-
Fig.16 Stage IB. T2w TSE image in sagittal orientation. High-signal-intensity cervical cancer (arrow) primarily involving the anterior cervix and the portio. Gel filling of the vagina
cal carcinoma as a highor intermediate-inten- sity lesion within the low-signal-intensity oval cervical stroma (Figs. 11, 16, 17, 18, and 19). Cervical cancer at this stage is fairly smoothly marginated and completely surrounded by low- signal-intensity cervical stroma. Occasional exophytic bulging of a stage IB tumor into the vagina or the parametrium may be mistaken for infiltration.
A large stage IB2 cervical carcinoma can obstruct the cervical canal and lead to hydrometra or hematometra. Hydroor serometra is suggested by a fluid collection in the uterine cavity showing hyperintensity in T2-weighted and low- signal-intensity in T1-weighted images, whereas a hematometra is characterized by high signal intensity in T2and T1-weighted images.
The rationale of using MR imaging at this stage of disease is to accurately assess tumor size, parametrial invasion, lower vaginal involvement, and lymph node metastases. Identification of this prognostic factors would preclude surgical treatment and is thus crucial for therapy planning (Freeman et al. 2013; Cheng et al. 2004; Kupets and Covens 2001).
2.3.4.3 Stage IIA
In stage IIA cervical cancer, infiltration involves up to two-thirds of the proximal vagina while sparing the lower third. On T2-weighted MR images, vaginal involvement is seen as a
142 |
F. Collettini and B. Hamm |
|
|
a |
b |
Fig. 17 Stage IB. (a, b) T2w TSE images in sagittal and transverse orientation. The cervical cancer is seen as a high-signal-intensity lesion within the cervix (arrows).
The cancer is surrounded by low-signal-intensity cervical stroma on both sagittal and transverse images. Accessory finding: Nabothian cysts
hyperintense segmental disruption or lesion in the otherwise low-signal-intensity vaginal wall. Infiltration of the anterior and posterior fornix and of the wall is best seen in sagittal orientation (Figs. 20, 21, 22, and 23). The radiologist interpreting the images must be aware that a large exophytic cervical cancer may lead to widening of the fornix and thus mimic vaginal infiltration. In such cases, opacification and distention of the vagina can be helpful. Similarly to stage IB, stage IIA is further subdivided into IIA1 (if the tumor is 4 cm or smaller in diameter) and IIA2 (for tumors greater than 4 cm in diameter). Stage IIA is further defined by the absence of parametrial invasion. Parametrial infiltration can be reliably excluded if the tumor is surrounded by a low- signal-intensity rim on transverse angulated T2-weighted images.
2.3.4.4 Stage IIB
Stage IIB cervical cancer is characterized by parametrial infiltration but without extension to the pelvic sidewall. Parametrial infiltration has important implications for the therapeutic approach. While gross parametrial invasion can be usually detected by experienced clinicians, early invasion usually remains undetected. Reported accuracy of clinical staging for detec-
tion of parametrial and pelvic side wall invasion amounts to only 29–53% (Hricak et al. 1988; Zand et al. 2007). MRI is the only noninvasive modality that allows adequate evaluation of parametrial infiltration with a reported sensitivity of 69%, specificity of 93%, and negative predictive values of 100% for depicting parametrial invasion (Zand et al. 2007). Sagittal and transverse T2-weighted images angulated perpendicular to the cervical canal are most suitable to evaluate parametrial infiltration. It is indicated by a disruption of the low-signal-intensity cervical stroma and tumoral extension into the parametria. Visualization of an uninterrupted rim of cervical stromal rim thicker than 3 mm (“hypointense rim sign”) reliably excludes parametrial infiltration with a specificity as high as 99% (Zand et al. 2007). The accuracy of MRI in the evaluation of parametrial invasion varies according to the tumor size, with 96% accuracy in small tumors and 70% in large tumors (Zand et al. 2007). Early microscopic parametrial infiltration must be suggested if high-signal-intensity tumor tissue shows irregular and unsharp margins and is disrupting the hypointense cervical stroma with no normal cervical stroma left that separates the tumor from the parametria. The most reliable MRI criterion of parametrial infiltration is the direct visualization

Cervical Cancer |
143 |
|
|
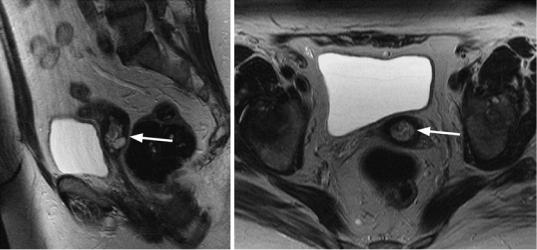
a b
c |
d |
Fig. 18 Stage IB. (a, b) T2w TSE images in sagittal and transverse orientation. High-signal-intensity lesion of the cervix (arrows) with preservation of low-signal intensity stroma around the tumor. (c, d) T1w TSE images in sagit-
tal and transverse orientation. No circumscribed cervical cancer is seen on the image obtained 1 min after Gd-DTPA administration. Accessory finding: uterine adenomyosis
of a tumor mass extending into the parametria (Figs. 24, 25, 26, and 27). Occasionally, the parametria may be invaded from below, through the paravaginal space. The anatomy of the true pelvis determines the further routes of spread of cervical cancer. Infiltration of the rectouterine or vesicouterine ligaments at their cervical attachments is seen on MR images as focal thickening. In rare cases, parametrial invasion can cause retraction with displacement of the cervix to the side of infiltration.
2.3.4.5 Stage IIIA
Stage IIIA tumor is established when there is involvement of the lower third of the vagina. As with stage IIA tumor, sagittal and oblique transverse T2-weighted sequences are most suitable to evaluate vaginal infiltration. Tumor infiltration is indicated by a hyperintense disruption and continuous or discontinuous thickening of the vaginal wall that extends to the lower third of the vagina. This stage is also associated with an increased risk of metastatic spread to the
