
Книги по МРТ КТ на английском языке / Advanced Imaging of the Abdomen - Jovitas Skucas
.pdf
14
metallic stents of benign esophageal strictures results in a high complication rate. Perforation and stent migration are not uncommon complications; stents have been passed per rectum or regurgitated. Nevertheless, in some patients temporary stenting of a benign esophageal stricture is useful. Covered expandable nitinol stents can be removed with a retrieval hook (31).
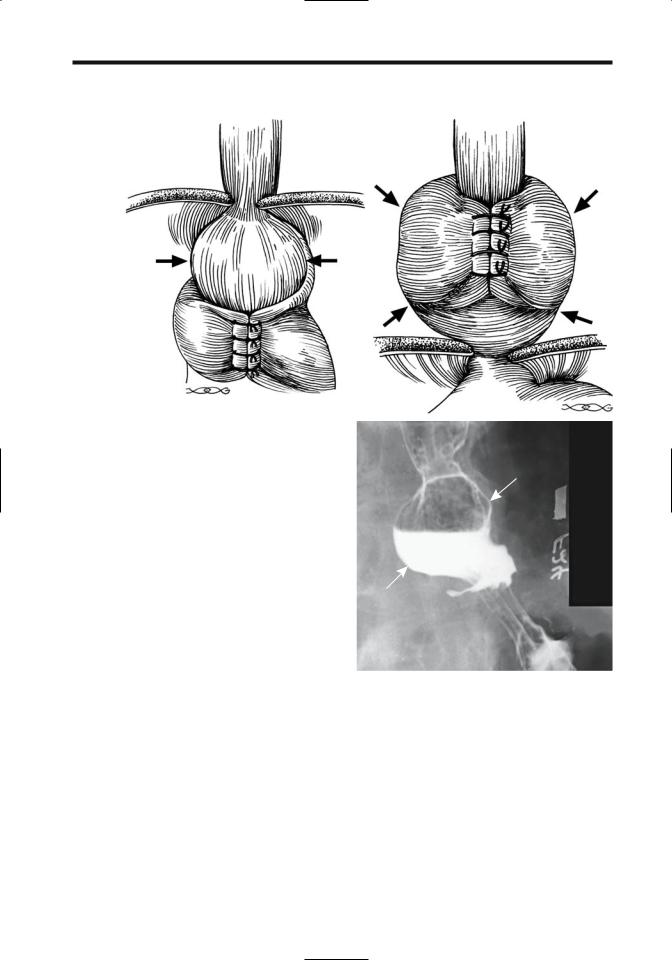
In many centers laparoscopic antireflux surgery has supplanted open surgery; laparoscopic and open fundoplications achieve similar results. Currently popular operations include the Nissen fundoplication (Fig. 1.8) and the Hill posterior gastropexy repair. Both have a similarly high success rate, although they are not complication free. Acute complications include esophageal or gastric perforation, gastric volvulus and an incarcerated intrathoracic hernia. Esophageal manometry reveals a considerable increase in lower esophageal sphincter resting pressure and sphincter length after fundoplication, and thus provides objective data of fundoplication effectiveness.
Pneumomediastinum detected shortly after laparoscopic fundoplication is probably of little or no significance; pneumothorax, on the other
ADVANCED IMAGING OF THE ABDOMEN
hand, is abnormal and should be investigated, keeping in mind that during a laparoscopic fundoplication the left pleura is entered and results in a pneumothorax (32).
Roughly 10% of patients have fundoplication failure and develop recurrent gastroesophageal reflux. Other complications include refractory dysphagia, intractable gas bloating, chest or abdominal pain, and incapacitating diarrhea, findings due to a tight repair, vagal nerve injury resulting in gastroparesis, and ulcerations. Although dysphagia improves in some patients, others require dilations or even reoperation. Acute dysphagia after a fundoplication usually implies a tight repair; later, esophageal stenosis should be suspected, possibly related to the diathermy dissection performed. Other complications include a slipped or disrupted fundoplication and recurrent hiatal hernia (Fig. 1.9). Unrecognized esophageal dysmotility accounts for occasional dysphagia,but this finding should be detected with preoperative imaging. A gastrobronchial fistula or esophagobronchial fistula is a rare complication. Computed tomography in one patient identified left lower lobe consolidation and left bronchial tree filling with contrast from a left subphrenic abscess, with a fistula confirmed by oral contrast (33).
Dilation for recurrent dysphagia in patients with a slipped fundoplication has a lower success rate than in those with an intact fundoplication.
Many children undergoing a fundoplication are neurologically impaired and thus prone to surgical complications. A fundoplication breakdown, recurrent hiatal hernia, or both are indications for a second antireflux operation (34); complications after a second Nissen fundoplication include bowel obstruction, wound infection, a tight wrap, and pneumonia. Long-term, only 72% of these children remained symptom free.
Figure 1.8. Prominent postoperative Nissen fundoplication. The distal esophagus is narrowed by an edematous fundal wrap.
Barrett’s Esophagus
Clinical
A Barrett’s esophagus consists of replacement of normal esophageal squamous epithelium by a specialized columnar epithelium, called heterotopic gastric mucosa. Such metaplasia is believed to be induced by chronic gastroesophageal reflux, esophagitis, and a unique
15
ESOPHAGUS
A
B
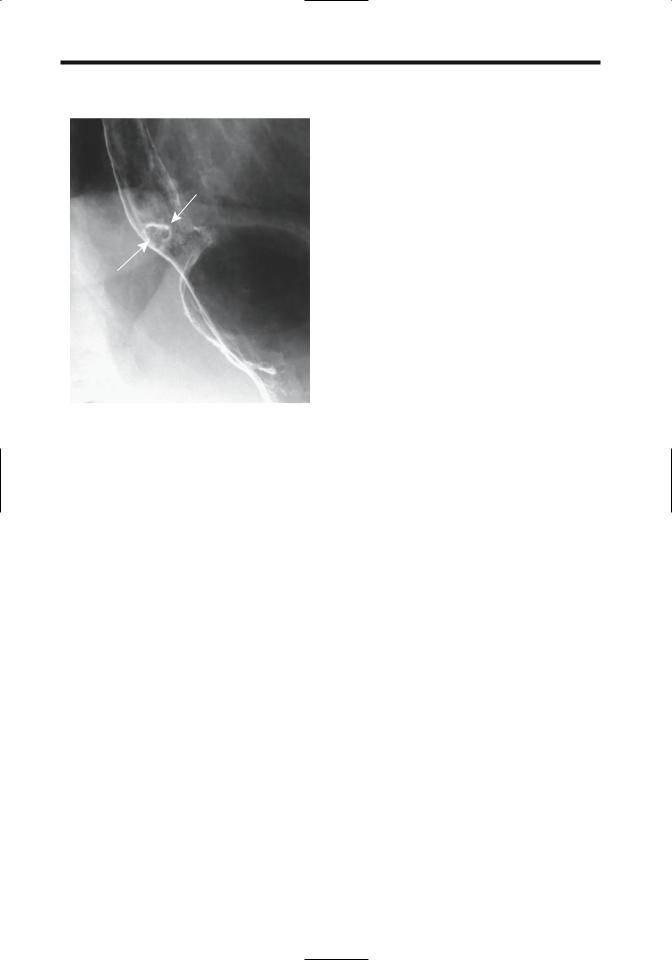
Figure 1.9. Complications of fundoplication. A: Part of the |
|
stomach (arrows) has herniated above the fundoplication, |
|
permitting reflux from this segment. B: The proximal stomach, |
|
including fundoplication, has herniated into the chest (arrows). |
|
C: Part of the stomach has herniated superiorly through the |
|
fundoplication. |
C |
type of healing, although this view is probably |
mucosa (36); all those positive in the esophagus |
an oversimplification; duodenogastric reflux |
were also positive in the stomach. The presence |
appears to be involved in some patients. A |
of H. pylori in the esophagus is related to pres- |
Barrett’s esophagus can develop after total gas- |
ence of gastric-type mucosa and of concomitant |
trectomy and esophagojejunostomy. It is more |
gastric H. pylori infection. |
often encountered in men and in Caucasians. |
Given the increasing survival of cystic fibrosis |
A familial occurrence is evident in some fami- |
patients and their propensity for gastro- |
lies. For some reason it is uncommon in Japan |
esophageal reflux, they appear to be at increased |
(35). |
risk for a Barrett’s esophagus. |
Does Helicobacter pylori infection play a role |
Occasionally heterotopic gastric mucosa is |
in a Barrett’s esophagus? In 73 patients with a |
encountered in the upper one third of the |
Barrett’s esophagus, H. pylori was detected in |
esophagus or even pharynx without other |
the esophagus in 15% and in 36% of gastric |
stigmata of Barrett’s esophagus, a condition |
16
believed by some to be congenital (37). Complications of such proximal heterotopic gastric mucosa include fistula formation and an adenocarcinoma.
Prevalence of Barrett’s esophagus is unknown because both imaging and endoscopy misses some of these lesions. Although at times Barrett’s esophagus has a characteristic appearance, mucosal biopsy is necessary for confirmation. Pathologically, the presence of esophageal gland ducts in columnar epitheliumlined mucosa is pathognomonic of Barrett’s esophagus but is not often sought.
A Barrett’s esophagus is either continuous in extent or patchy and surrounded by normal esophageal mucosa. Most often Barrett’s esophagus is located just proximal to the lower esophageal sphincter. Such complications of Barrett’s esophagus as ulceration, stricture, dysplasia, and cancer tend to be less prevalent in a short-segment Barrett’s.
A Barrett’s esophagus is considered premalignant, with an intermediate stage being dysplasia. An ongoing concern is biopsy sampling error and ability to differentiate low-grade dysplasia from high-grade dysplasia, with the latter tissue being at risk for malignant degeneration. Grading of dysplasia is subject to observer variability. The presence of positive tumor markers such as p53, c-erb-2, proliferating cell nuclear antigen (PCNA), and carcinoembryonic antigen (CEA) or the existence of aneuploidy is used by some to gauge the risk for progression to malignancy, but no firm criteria are available.
Estimates of adenocarcinoma prevalence in patients with Barrett’s esophagus vary widely. In a Spanish study, an adenocarcinoma developed at an incidence of 1 per 104 Barrett’s esophagus per year (38), while at a Veterans Administration Medical Center in Tucson, Arizona, it was 1 per 208 Barrett’s esophagus per year (39). Severe dysplasia commonly surrounds a carcinoma. Some studies suggest that patients with an esophageal adenocarcinoma, presumably arising from Barrett’s esophagus, are not at higher risk of developing extraesophageal malignancies, but other reviews have reached the opposite conclusion, finding that patients with Barrett’s esophagus are at increased risk of colon cancer.
Occasionally Barrett’s esophagus regresses after medical therapy, but such results are inconclusive.
ADVANCED IMAGING OF THE ABDOMEN
Imaging
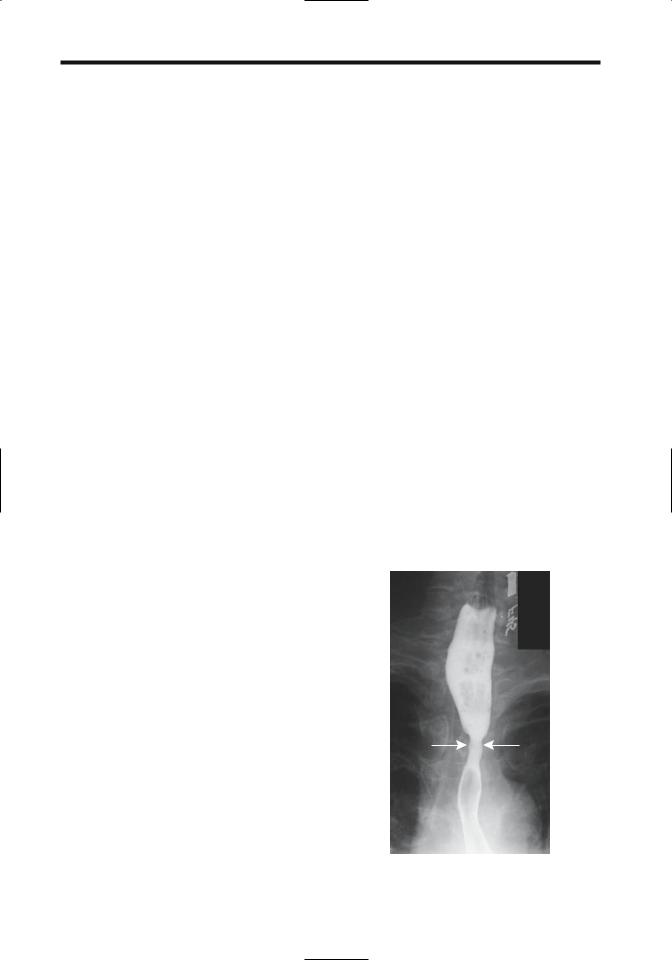
A typical barium study of a Barrett’s esophagus reveals an irregular or reticular region of barium coating,ulcers,and strictures (Fig. 1.10). Involvement commonly is close to the squamocolumnar junction. The reticular appearance tends to be rather subtle, and a high-quality double-contrast esophagram is necessary to detect these lesions. At times deep ulcers develop, a finding not generally seen in uncomplicated reflux esophagitis.
A double-contrast esophagram in patients with short-segment Barrett’s esophagus revealed hiatal hernias in 90%, gastroesophageal reflux in 80%, reflux esophagitis in 35%, and peptic scarring or strictures in 55% (40); a reticular pattern was not seen in these patients.
Endoscopic US shows that the mucosal second hypoechoic layer is significantly thicker in Barrett’s patients than in a normal esophagus (41); Barrett’s esophagus can be diagnosed with a sensitivity approaching 100% and specificity of 86% if the mucosa hypoechoic layer is thicker than the first hyperechoic layer. More common is detection of focal esophageal wall thickening; such thickening is also found with some carcinomas, and endoscopic US cannot distinguish
Figure 1.10. Barrett’s stricture (arrows). Adenocarcinomatous transformation is in the differential diagnosis.
17
ESOPHAGUS
between benign and malignant causes of wall thickening.
Drug-Induced Inflammation
A specific etiology for drug-induced esophagitis is not known. One postulate suggests that the weak caustic action of many drugs during their stasis in the esophagus results in localized corrosive injury. Numerous drugs are implicated in esophagitis and lead to ulcerations. Common ones include tetracycline derivatives and nonsteroidal antiinflammatory agents. Typically, a pill lodges in the esophagus at sites of normal narrowing such as the aortic arch or proximal to a stricture or due to lack of propulsion. Alendronate, used to treat osteoporosis in postmenopausal women, has led to multiple ulcers and strictures resistant to dilation.
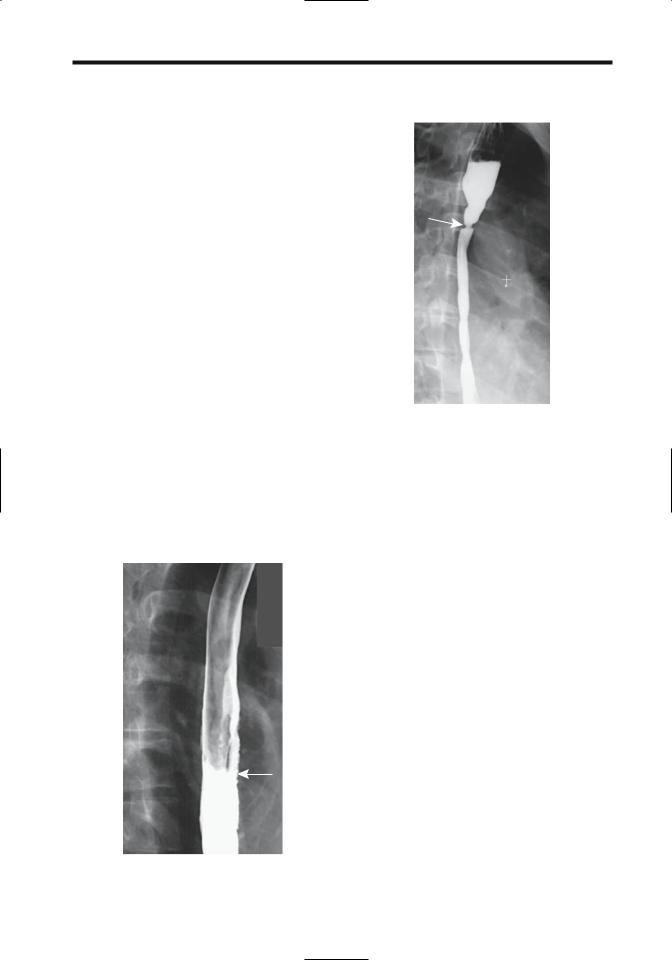
These ulcers tend to be multiple, often shallow, and clustered at one site. Surrounding inflammation, manifesting as thickened folds, is common. An occasional one is large, presumably due to coalescence of smaller ulcers (Fig. 1.11). These ulcers heal readily once the incriminating agent is withdrawn, although an occasional one progresses to esophageal perforation.
Figure 1.11. Aspirin-induced focal esophagitis. Thickened folds and subtle ulcers are present in the mid-esophagus (arrow).
Figure 1.12. Sequela of lye stricture as a child. An esophagram reveals a long stricture involving most of the esophagus. A proximal web-like stricture (arrow) required periodic balloon dilation.
Thermal/Corrosive Injury
Acute thermal injury develops after ingestion of hot substances. Ingestion of solid alkali produces mostly oropharyngeal damage. Liquid alkali, such as drain cleaners, and acid ingestion, such as hydrochloric acid, damage both the esophagus and the stomach and occasionally even extend into the duodenum. Necrosis ensues, and at times it is massive. Unless perforation develops, the acute phase gradually subsides within a week or so,and strictures,at times bizarre in appearance, begin to form. Previous corrosive injury is associated with an increased risk of carcinoma.
On a long-term basis, some type of esophageal dysmotility persists in most patients who ingest corrosives, most often consisting of nonperistaltic low-amplitude contractions. Long strictures are common, at times gradually progressing and manifesting years later (Fig. 1.12).
Most patients with corrosive injury are managed by gastroenterologists who prefer endoscopy rather than radiographic contrast studies to evaluate underlying damage. Lye ingestion is one of the causes of a dark-

18
ADVANCED IMAGING OF THE ABDOMEN
pigmented or black esophagus seen during endoscopy.
Crohn’s Disease
In the gastrointestinal tract, the esophagus is least likely to be involved by Crohn’s disease. When present, dysphagia, odynophagia, and, at times, bleeding develop. Most patients also have gastric and distal ileal involvement.
The most common appearance consists of aphthae. Occasionally these aphthae enlarge and linear ulcers develop. These ulcers have evolved into deep, intramural tracts parallel to the esophageal lumen. A rare Crohn’s esophagus presents as a polyposis. Rarely, severe involvement leads to irregular ulcerations and an imaging appearance mimicking other severe inflammation.
Crohn’s involvement of the esophagus is one of the more uncommon causes of esophageal stricture or an esophagopulmonary fistula (42).
Phlegmonous Esophagitis
Phlegmonous esophagitis is rare. An infection usually extends from the stomach.
Severe esophageal infection or ischemia could result in esophageal pneumatosis, but in practice it is a rare finding. Occasionally esophageal pneumatosis develops after acute gastric dilatation (43).
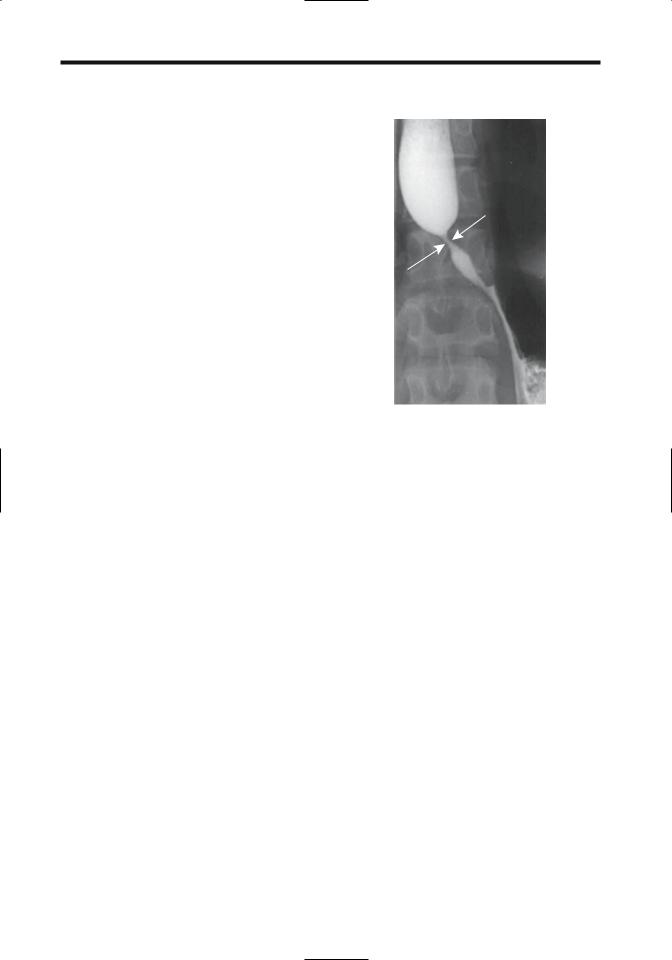
Tuberculosis
Primary esophageal tuberculosis is rare. More common is esophageal involvement secondary to extension from an adjacent structure, such as carinal lymph nodes (Fig. 1.13). Clinically, dysphagia and odynophagia predominate. A rare esophageal tuberculosis evolves into an intramural abscess (44). Anecdotal reports describe spontaneous esophageal perforation, and a spontaneous esophageal fistula/sinus tract with no known underlying etiology should suggest tuberculosis.
Radiographic findings vary considerably and include nodularity, stricture, ulcer, and fistula. An intraluminal septum probably represents a fistula with secondary luminal recommunication. Computed tomography reveals mediastinal or other adjacent adenopathy.
A biopsy from a site of ulceration or mass often simply shows epithelioid cell granulomas.
Figure 1.13. Tuberculous sinus tract between esophagus and carinal lymph nodes (arrow) in a patient with dysphagia. Primary disease was in the lymph nodes.
At times culture of the biopsy material reveals
Mycobacterium tuberculosis, but such cultures are not commonly performed.
Candidiasis
Although occasionally developing without an underlying cause, esophageal candidiasis typically evolves in a setting of immunosuppression, malignancy, diabetes mellitus, debilitation, scleroderma, or drug use. Oral thrush is not always identified. Dysphagia is a common presentation, with or without odynophagia.
A double-contrast barium study differentiates most candida esophagitis from other esophagitides. Varying-size plaques, tending to align to the esophageal longitudinal axis, are a typical appearance of candidiasis (Fig. 1.14). With progression, these plaques coalesce; some become undermined and the appearance is that of a shaggy, irregular outline. A foamy esophagus has been described on a doublecontrast esophagram (45); it consists of innumerable small, round gas bubbles mixed with barium on top of the barium column. Ulcers are uncommon early but develop with plaque sloughing.

19
ESOPHAGUS
Figure 1.14. Candida esophagitis. The esophagus has a shaggy, irregular outline.
Viral Esophagitis
Herpes simplex virus type I esophagitis develops most often in immunocompromised patients. An esophagram typically reveals welldefined ulcers in otherwise normal-appearing mucosa. These ulcers range from punctate to round or, rarely, linear.
Cytomegalovirus and HIV-induced ulcers tend to be large and shallow. The imaging appearance with both is similar, and biopsy is necessary for differentiation.
Chronic Granulomatous Disease
Chronic granulomatous disease is an inherited disease manifesting in childhood and characterized by recurrent bacterial or fungal infections. The primary defect is a neutrophil granulocyte dysfunction that suppresses the body’s ability to kill phagocytosed microorganisms. This condition rarely involves the esophagus, although an occasional child develops esophageal narrowing. Biopsy simply revealed nonspecific inflammation.
This entity differs from the rare chronic granulomatosis found in adults (discussed in Chapter 14).
Eosinophilic Esophagitis
Eosinophilic esophagitis is a rare cause of dysphagia, generally detected in the young. Isolated esophageal involvement does occur, but more common is disseminated disease. Dysphagia and chest pain are typical presentations. An allergic history is common and many of these patients have a peripheral eosinophilia.
Imaging does not play a direct role in the diagnosis but serves primarily to exclude complications, such as strictures and other conditions.
Other
Chronic dysphagia but without symptoms of reflux has been described in patients developing localized esophageal strictures (46); histology reveals esophageal mucosal blistering but no significant inflammation and no concurrent cutaneous or mucous lesions. The authors called this entity chronic esophagitis dissecans.
Histoplasmosis
Primary esophageal histoplasmosis is rare and occurs mostly in immunocompromised patients. More likely esophageal involvement is secondary to one of two circumstances: First, with mediastinal histoplasmosis, resultant adenopathy and inflammation lead to esophageal obstruction and dysphagia. Second, esophageal ulcers and nodules develop in a setting of disseminated histoplasmosis. A histoplasmosis-associated stricture is rare.
Biopsy reveals intracellular histoplasmosis.
Behçet’s Syndrome
Behçet’s syndrome involving the esophagus is rare. The few reported patients presented with esophageal ulcers varying in depth (Behçet’s syndrome is discussed in Chapter 17).
Radiation
Clinically evident radiation esophagitis is not common. Patients also receiving Adriamycin or actinomycin-D have a considerably lower threshold for radiation esophagitis.
20
ADVANCED IMAGING OF THE ABDOMEN
Patients undergoing concurrent chemoand radiotherapy for lung cancer have a considerably lower threshold for radiation esophagitis which is confined to the radiation field (47); esophagitis was more common in the low-dose chemotherapy group than in those receiving a larger dose.
The imaging appearance ranges from isolated ulcers, usually shallow, to eventual long strictures in the radiation field.
Sarcoidosis
Sarcoidosis typically involves lungs, lymph nodes, and spleen, with gastrointestinal involvement being less common. The hallmark of sarcoidosis is the presence of noncaseating granulomas, although similar histologic findings are found in a number of disorders. In general, single-organ involvement is uncommon and should not be attributed to sarcoidosis. A possibility of sarcoidosis (and its therapy) predisposing to lymphoma has been raised, presumably via an immune system pathway. Sarcoidosis has preceded lymphoma by months or years.
Sufficient mediastinal sarcoid adenopathy can compress and narrow the esophagus lumen. A barium study typically reveals a smooth and narrowed esophageal lumen. Subcarinal adenopathy often splays the right and left main stem bronchi. In most patients esophageal motility is normal. Manometry occasionally reveals nontransmitted contractions and a spastic lower esophageal sphincter. The rare primary esophageal sarcoidosis presents as a focal, circumferential stricture (Fig. 1.15).
Fibrosis
Esophageal fibrosis and fibrosis-associated strictures are a common end point for a number of conditions (Table 1.3), and these are discussed in their appropriate sections. In distinction to other parts of the gastrointestinal tract, the relative smoothness of an esophageal stricture is an insensitive guide in distinguishing a benign from a malignant stricture. Also, not all esophageal narrowings represent a stricture; for instance, the distal esophageal narrowing in achalasia is mostly spasm.
Figure 1.15. Esophageal sarcoidosis manifesting as a circumferential, smooth stricture (arrows).
Extensive mediastinal fibrosis does lead to esophageal stricture. Generally these strictures have a smooth appearance and tapering margins. Self-expanding stents have been helpful in relieving acute dysphagia in these patients.
Tumors
Nonneoplastic
Sebaceous Glands
Normally sebaceous glands do not exist in the esophagus, although ectopic sebaceous glands have been described. They vary in size; some appear as irregular, lobulated nodules, while a rare patient has multiple rounded polyps arranged in rows.
Histology is diagnostic for these submucosal glands.
Fibrovascular Polyp
Most giant intraluminal esophageal polyps are fibrovascular in origin. An occasional one is a leiomyoma, hamartoma, or some other difficult to classify tumor.

21
ESOPHAGUS |
|
Table 1.3. Etiologies of fibrotic esophageal strictures |
|
|
|
Condition |
Comments |
|
|
Reflux esophagitis |
Both acid and alkali reflux result in strictures, usually in distal third |
Barrett’s esophagus |
Most strictures are in middle or distal third |
Drug induced |
Most common in mid-esophagus |
Thermal/corrosive |
Most strictures are long and in distal segment |
Crohn’s disease |
Strictures tend to be smooth and vary in length |
Phlegmonous |
Involves distal segment and usually extends into stomach |
Infectious |
Strictures result from chronic infection |
Chronic granulomatous disease |
Fibrosis is secondary to recurrent bacterial or fungal infections |
Chronic esophagitis dissecans |
A rare cause of esophageal strictures |
Radiation |
Strictures correspond to radiation port and tend to be smooth in outline |
Mediastinal fibromatosis |
Esophagus tends to be extensively involved |
Sarcoidosis |
Usually secondary to mediastinal sarcoidosis |
Plummer-Vinson syndrome |
Appearance more web-like rather than a fibrotic stricture |
Epidermolysis bullosa |
Ulcerations lead to fibrotic strictures |
Pemphigoid |
Blistering results in web-like appearance, at times evolving into strictures |
Prolonged nasogastric intubation |
Long distal esophageal strictures |
Intramural (pseudo)diverticulosis |
Distal esophageal strictures are probably due to reflux esophagitis |
|
|
Most fibrovascular polyps originate in the proximal one third of the esophagus, originate in the submucosa, are covered by squamous epithelium, and consist of fibrosis, fat, and stromal tissue. Most present with either lumen obstruction or bleeding. They obstruct when large. Some develop a long pedicle and prolapse, even to the point of laryngeal obstruction. Occasionally CT and MR identify predominantly fat (48).
Being rather mobile, during a barium study these polyps superficially mimic a bolus of food.
Hemangioma
Esophageal hemangiomas are uncommon. Most appear as sessile polyps. Computed tomography reveals marked contrast enhancement. One was hypoechoic on endoscopic US, was confined to the submucosa, and adjacent muscularis propria appeared intact (49).
Heterotopic Pancreas
The term choristoma is occasionally used to describe a tumor-like mass of normal tissue in an abnormal location. A heterotopic pancreas is one such tumor.
Obvious heterotopic pancreatic tissue is rare in the esophagus, but intramucosal pancreatic acinar-like cells are not. These pancreatic acinar
cells tend to be located on either side of the squamocolumnar junction, but they do not represent ectopic pancreatic tissue.
Benign Neoplasms
Papilloma
The majority of squamous cell papillomas occur in the distal esophagus and most are asymptomatic. Some papillomas are associated with mucosal injury and subsequent regeneration. They are not considered premalignant. They tend to be misdiagnosed as mucosal tags or inflammatory polyps if only small biopsy specimens are available, but the pathologist should suggest a correct diagnosis if papillary projections are identified. Radiologically, most are small, range from smooth to slightly irregular, and vary in size (Fig. 1.16).
Leiomyoma
A leiomyoma is the most common esophageal tumor found at autopsy. Most are intramural in location, single, small, and not detected by imaging. Most are discovered incidentally, and the larger ones result in dysphagia. Most occur in adults.
A rare leiomyoma grows mostly intraluminal, at times even becoming pedunculated, thus suggesting a muscularis mucosa origin. An occa-
22
ADVANCED IMAGING OF THE ABDOMEN
Figure 1.16. Squamous papilloma close to the gastroesophageal junction (arrows).
sional one mimics a fibrovascular polyp, especially if originating in the proximal esophagus. One pedunculated leiomyoma extended 20cm in a dilated esophagus containing retained foreign material (50); the overall appearance suggested achalasia.
Precontrast, leiomyomas tend to be close to isointense; they enhance homogeneously postcontrast, except for larger ones containing necrosis.
Endoscopic US of a plexiform leiomyoma showed a sharply marginated, hypoechoic intramural tumor containing internal linear echoes (51). Endoscopic US should differentiate whether a leiomyoma originates from muscularis mucosa or muscularis propria; endoscopic lumpectomy is possible for those originating from muscularis mucosa.
Diffuse esophageal leiomyomatosis occurs in X-linked Alport’s syndrome, an inherited dominant trait caused by specific gene mutations, and, in fact, diffuse leiomyomatosis and esophageal involvement are often the first manifestations of Alport’s syndrome. Progressive dysphagia starting in childhood is typical.
A barium esophagram in leiomyomatosis reveals smooth esophageal narrowing. Computed tomography and endoscopic US identify diffuse esophageal wall thickening.
Malignant Neoplasms
Pharyngeal Tumors
Pharyngeal malignancies originate in any of the three pharyngeal compartments: nasopharynx, oropharynx, or hypopharynx. Most are squamous cell carcinomas, with a minority of lymphomas, adenoid cystic carcinomas, and rare undifferentiated carcinomas. Pharyngeal sarcomas are rare.
Direct visualization continues to be the mainstay of tumor detection, while pharyngography has been supplanted by CT and MRI in evaluating tumor spread. Neck MRI is especially helpful due to its enhanced soft tissue contrast.
Esophageal Carcinoma
Among patients with esophageal carcinoma seen at the Cleveland Clinic Foundation between 1987 and 1994, 74% had an adenocarcinoma and 26% a squamous cell carcinoma (52); no differences existed between the two groups in age, prior gastric surgery, smoking, or alcohol use, but significant risk factors for an adenocarcinoma were male gender, white race, distal cancer location, and the presence of Barrett’s esophagus.
Clinical
Squamous Cell Carcinoma: Esophageal squamous cell carcinoma shows considerable regional variation in prevalence. Both tobacco and alcohol use are predisposing risk factors in the Western world, but these do not appear to play a major role in regions of the world where this cancer is especially prevalent. In the United States, tobacco plays a greater role in esophageal squamous cell carcinoma than in adenocarcinoma and is a more prominent factor in women than men (53). Human papillomavirus appears to have a role in carcinogenesis in geographic regions with a high prevalence of this cancer.
A patient with an esophageal squamous cell carcinoma presented with paraneoplastic glomerulonephritis and nephrotic syndrome (54); such an autoimmune phenomenon appears to be induced by tumor antigen

23
ESOPHAGUS
inhibition. The sign of Leser-Trelat (multiple verrucous papules) is also associated with a rare squamous cell esophageal carcinoma (55).
Dysphagia for solid foods is the most common presentation but is a late occurrence.
An association exists between esophageal dysplasia and both esophageal carcinoma and head and neck carcinomas. Patients who have had a prior partial gastrectomy for peptic ulcer disease also appear to be at increased risk. An occasional carcinoma is linked to prior radiation therapy to this region. Increased prevalence is found in patients with achalasia, Plummer-Vincent syndrome, a caustic stricture, or tylosis (keratopalmar keratosis), an autosomal condition.
Simultaneous esophageal squamous cell carcinoma and gastric adenocarcinoma have developed, but whether these have been by chance is conjecture. In a rare patient intramural pseudodiverticulosis is associated with an esophageal carcinoma.
Esophageal squamous cell carcinoma exhibits considerable variability throughout the world. It is one of the leading causes of cancer death in Asia, with an especially high prevalence in northern Iran and northern China. Another focus of high prevalence is found among Zulu and Bantu people in South Africa. In Shanghai, esophageal cancer rates have decreased more than 50% over an 18-year period ending in 1989 (56), in the United States an increase is found among black men, while in Scotland, both adenocarcinoma and squamous carcinoma have been increasing both in men and women.
Adenocarcinoma: Discussed here are adenocarcinomas arising both in the esophagus and in the gastric cardia (at the gastroesophageal junction). Prior literature debated whether the latter tumors should be considered esophageal or gastric in origin, but from a clinical viewpoint little justifies their separate consideration; the resultant surgical approach is similar.
Extensive associated dysplasia is common surrounding an esophageal adenocarcinoma. Many of these patients have a long history of gastroesophageal reflux, and gastric content has thus been implicated in carcinogenesis, but a specific carcinogen has not been identified. Bile and pancreatic juice reflux have also been implicated. No significant association exists between H. pylori infection and carcinoma of the
gastroesophageal junction; this is in distinction to a significant association between H. pylori infection and other gastric adenocarcinomas.
Prevalence of esophageal and gastric cardia adenocarcinoma is increasing in the Western world. Data from the Surveillance, Epidemiology, and End Results (SEER) study in the United States reveal that in white males the incidence of esophageal adenocarcinoma increased >350% since the mid-1970s and currently surpasses squamous cell carcinoma (57); an increase also occurred in black males but was considerably lower.
Not all of these adenocarcinomas develop in a Barrett’s esophagus. Barrett’s esophagus patients tend to have a better prognosis after surgery, probably because reflux and similar symptoms result in an earlier diagnosis.
These tumors commonly invade the gastric cardia. A rare esophageal adenocarcinoma first manifests as a metastasis.
Small Cell Carcinoma: Primary small cell carcinoma, morphologically indistinguishable from its lung counterpart, is rare in the esophagus. Pathologically these tumors are divided into oat-cell and non–oat-cell varieties. These are aggressive tumors with a poor prognosis, although radiation therapy and chemotherapy does prolong survival.
These tumors vary in size from small mucosal lesions to large fungating masses. Extensive intrathoracic and intraabdominal adenopathy is not uncommon on initial presentation. Imaging studies tend to be similar to those seen in patients with a squamous cell carcinoma. Barium studies reveal a smoothly marginated, sessile, ulcerated tumor located inferior to the carina (58).
A rare association with celiac disease has been raised (59).Also, a rare patient with a small cell esophageal carcinoma has a synchronous squamous cell carcinoma.
Adenoid Carcinoma: An esophageal adenoid cystic carcinoma is rare. They tend to be rather aggressive.
Pathology
Esophageal lymphatics consist of a submucosal network draining into regional lymph nodes.An esophageal malignancy can thus spread readily both longitudinally and circumferentially.
